Imagine getting a generic version of your blood pressure medication - the same active ingredient, same price - but knowing exactly whether it will work for you or put you at risk. That’s no longer science fiction. Thanks to AI and pharmacogenomics, online pharmacies are starting to deliver personalized drug recommendations based on your genes. This isn’t about fancy brand-name drugs. It’s about making the cheapest, most common pills work better - and safer - for you.
What Is Pharmacogenomics (PGx)?
Pharmacogenomics sounds complicated, but it’s simple in practice: it’s how your genes affect how your body handles drugs. Two people can take the same pill, and one gets relief while the other gets sick. Why? Because of small differences in their DNA. Some people break down drugs too fast. Others break them down too slow. These differences are tied to specific genes, especially in the CYP450 enzyme family - your body’s main drug-processing system.
For example, if you’re a CYP2D6 ultrarapid metabolizer, a standard dose of codeine might turn into too much morphine, causing dangerous breathing problems. If you’re a poor metabolizer, clopidogrel (a common blood thinner) might not work at all. These aren’t rare edge cases. About 20% of people have at least one genetic variation that affects how they respond to common medications.
How AI Makes PGx Practical
For years, PGx testing existed - but it was slow, expensive, and hard to interpret. A pharmacist might spend 20 minutes reading a genetic report. Most clinics didn’t bother. AI changed that.
A 2024 study in the Journal of the American Medical Informatics Association showed an AI system using GPT-4, trained on official clinical guidelines (CPIC), could interpret PGx results in 2.3 seconds with 89.7% accuracy. That’s better than most human experts. The system doesn’t just say “you’re a slow metabolizer.” It explains: “Based on your CYP2C19 gene, this drug won’t work well. Try this alternative. Here’s why.”
What’s more, it translates jargon into plain language. In the same study, 92% of patients said the AI’s explanation made sense. Only 45% understood the standard clinical report. That’s huge. If you can’t understand why a drug was chosen, you won’t take it - or you’ll stop taking it.
Why This Matters for Online Pharmacies
Online pharmacies sell mostly generics. They rely on volume, low prices, and convenience. But they’re also where people get their prescriptions filled without seeing a doctor. That’s a risk. A generic statin might work for 80% of people - but for the other 20%, it could cause muscle damage or liver issues.
Now, imagine this: You order your cholesterol pill online. Before shipping, the pharmacy asks: “Have you had a PGx test?” If you have, they check your results. If not, they offer a $15 at-home cheek swab kit. Within 48 hours, their AI analyzes your data and says: “Your gene variant means this generic simvastatin could cause side effects. We’re sending you rosuvastatin instead - same effect, safer for you.”
This isn’t hypothetical. Mayo Clinic’s 2022 pilot reduced adverse drug events by 22% in cardiac patients using AI-guided PGx. A hospital in Florida cut consultation time by 12.7 minutes per patient. These are real savings - in time, money, and hospital visits.
How It Works Behind the Scenes
Most AI-PGx systems use something called retrieval-augmented generation (RAG). Think of it like a super-smart librarian. The AI doesn’t guess. It pulls answers from trusted sources: CPIC guidelines, PharmGKB databases, peer-reviewed studies. Then it combines that with your genetic data - like a variant in your SLCO1B1 gene affecting statin absorption - and gives you a clear recommendation.
These systems connect to electronic health records (EHRs) through secure APIs. If you’ve had a PGx test done at a hospital, that data can flow automatically to your online pharmacy. No manual entry. No errors. And because they use federated learning, your raw DNA data never leaves your provider’s secure system. Only the interpretation - “high risk for side effects” - gets shared.
Performance is strong. The GPT-4-based system handled 1,200 users at once with less than 5% drop in accuracy. It works on mobile, tablet, or desktop. And it’s fast: under 2 minutes per case, compared to 15-20 minutes for manual review.
What’s Missing - And What’s Risky
It’s not perfect. AI can hallucinate. In the JAMIA study, 3.2% of AI responses had clinically significant errors. One Reddit user reported the system missed a CYP2D6 ultrarapid metabolizer status for codeine - a potentially deadly oversight in a child. That’s why every recommendation still needs a human check, especially for high-risk drugs.
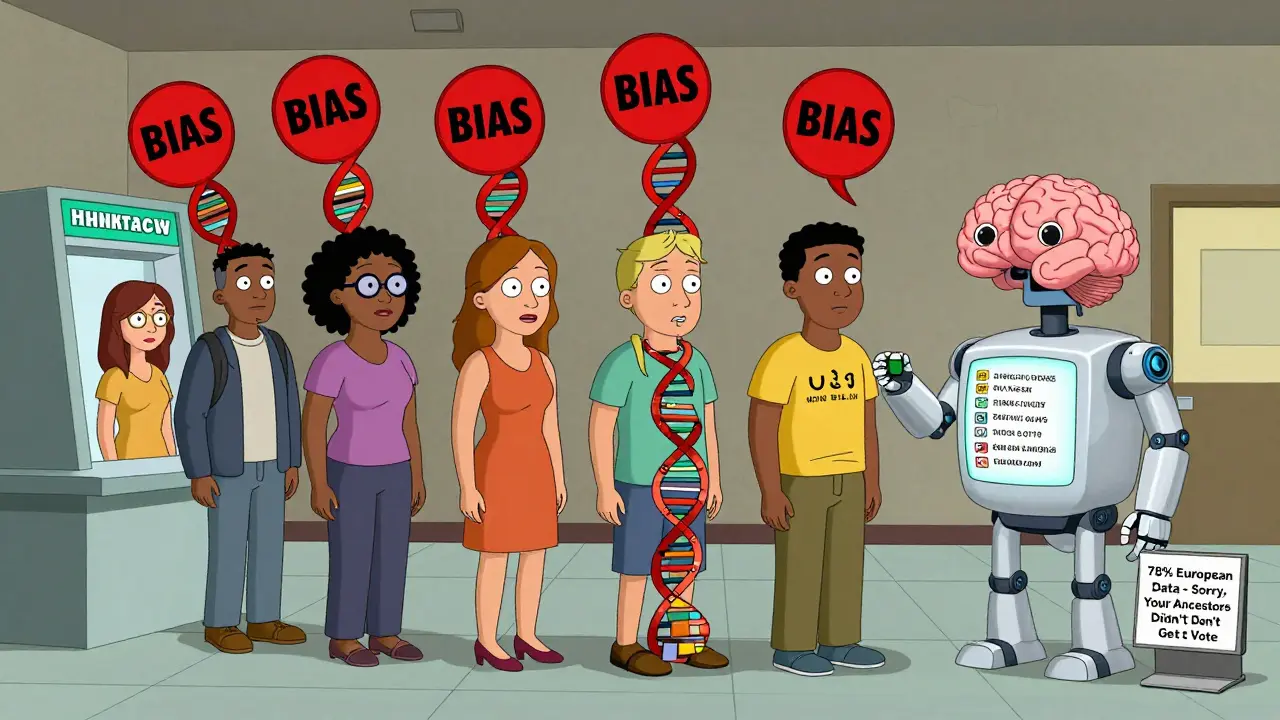
Another problem? Bias. Current PGx databases are 78% based on European ancestry data. But only 16% of the world’s population is European. That means the AI might give inaccurate advice to people of African, Asian, or Indigenous descent. A 2023 study in Cell Genomics found that non-European patients were 3x more likely to get wrong drug recommendations because the system had never seen their genetic patterns before.
Also, AI can’t read raw DNA yet. You need a lab report that says “rs12345678: GG.” You can’t just spit into a vial and send it to an online pharmacy - not yet. That’s still a gap.
Who’s Leading the Way?
Big players are moving fast. Google Health partnered with Mayo Clinic in 2022. Deep Genomics, a startup that raised $150 million in March 2024, is building AI models to predict how drugs interact with your proteins. The FDA cleared the first AI-PGx tool - GeneSight Psychotropic - in February 2023 for depression meds.
But the real shift is happening quietly. Major EHRs like Epic and Cerner now have built-in PGx modules. InterSystems, a healthcare data platform, developed algorithms that auto-suggest alternative drugs based on genetic data. And in April 2024, the NIH launched a $125 million initiative to fix bias and build transparent AI models for PGx.
Online pharmacies aren’t waiting. A 2023 KLAS report found that 68% of U.S. hospitals with 500+ beds now use some form of PGx. Only 22% use AI - but that’s growing fast. By 2027, experts predict 45% of academic medical centers will combine PGx with polygenic risk scores - giving you not just drug safety, but long-term disease prevention.
What You Can Do Today
You don’t need to wait for your pharmacy to catch up. If you’re on any long-term medication - statins, antidepressants, blood thinners, painkillers - ask your doctor for a PGx test. Many insurance plans cover it now. The test costs $100-$250 out of pocket.
Once you have your results, upload them to your pharmacy’s portal. If they don’t have an AI system yet, share the report with your pharmacist. Most will review it manually. You can also use free tools like PharmGKB’s public database to look up your gene variants and see what they mean.
And if you’re ordering generics online? Choose pharmacies that mention PGx integration. Look for phrases like “personalized drug matching” or “genetic safety check.” These aren’t marketing buzzwords anymore - they’re safety features.
The Bottom Line
AI and pharmacogenomics aren’t about making drugs more expensive. They’re about making the cheapest drugs work better. For the first time, generic medications can be truly personalized. No more guessing. No more trial and error. Just smarter, safer, faster choices.
The technology is ready. The data is there. The question isn’t whether this will happen - it’s how fast your pharmacy will catch on.



Natasha Bhala
February 8, 2026 AT 04:39Gouris Patnaik
February 8, 2026 AT 21:01Jesse Lord
February 9, 2026 AT 11:10AMIT JINDAL
February 11, 2026 AT 00:19Catherine Wybourne
February 11, 2026 AT 22:18Ashley Hutchins
February 12, 2026 AT 15:13Lakisha Sarbah
February 14, 2026 AT 10:49Marcus Jackson
February 14, 2026 AT 21:46