Anticholinergic Burden Calculator
Calculate Your Anticholinergic Burden
Your Current Medications
Results
Important: This tool calculates your total ACB score based on common medications. Always discuss with your doctor before making any medication changes.
When you’re prescribed a tricyclic antidepressant like amitriptyline or nortriptyline for depression or chronic pain, you’re not just getting a mood stabilizer. You’re also getting a powerful blocker of acetylcholine - a brain chemical critical for memory, focus, and heart rhythm. This hidden effect is called anticholinergic burden, and it’s one of the most overlooked dangers in modern prescribing. For people over 50, especially those taking multiple medications, this burden can quietly erode memory, mimic dementia, and put the heart at serious risk - all without being flagged as a side effect by most patients or even some doctors.
What Exactly Is Anticholinergic Burden?
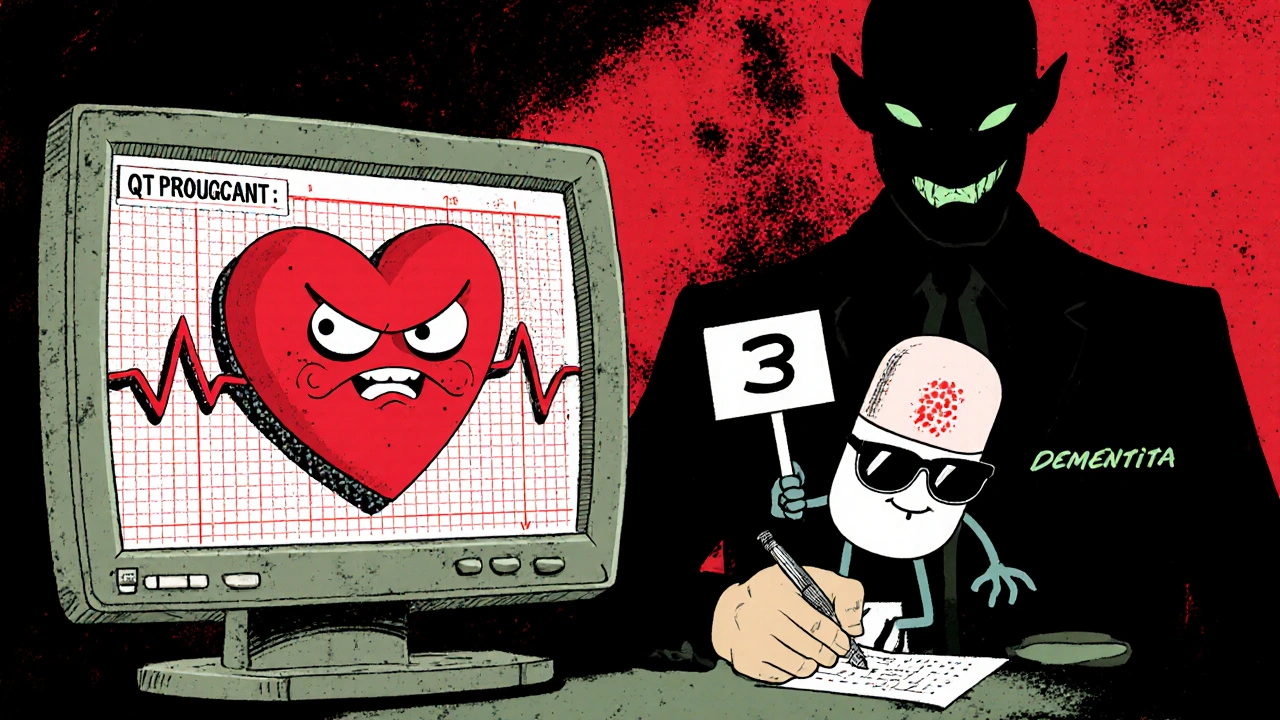
Anticholinergic burden isn’t about one drug. It’s the total effect of all the medicines in your system that block acetylcholine. Think of it like filling a bucket with water. Each pill you take - whether it’s an antidepressant, an antihistamine for allergies, or a bladder medication - adds a splash. Over time, the bucket overflows. The Anticholinergic Cognitive Burden (ACB) Scale is the tool doctors use to measure this. It rates drugs from 1 (mild) to 3 (high). Tricyclic antidepressants? They all score a 3. That’s the highest possible. Amitriptyline, doxepin, imipramine - they’re in the same dangerous category as diphenhydramine (Benadryl) and oxybutynin (for overactive bladder).Here’s what that means in real terms: if you’re taking just one TCA, your ACB score is already 3. Add a nighttime sleep aid with diphenhydramine? That’s 6. Now throw in an antihistamine for hay fever? You’re at 9. Research shows that an ACB score of 3 or higher doubles your risk of developing dementia over seven years. And here’s the kicker - the damage isn’t always reversible. Even after stopping the drugs, some cognitive decline sticks around.
Why TCAs Are So Problematic
Tricyclic antidepressants were groundbreaking in the 1960s. They worked where nothing else did. But they were never meant to be long-term solutions. Their mechanism is blunt: they stop serotonin and norepinephrine from being reabsorbed - good for mood. But they also slam the brakes on acetylcholine receptors - bad for everything else. Unlike modern SSRIs or SNRIs, which barely touch acetylcholine, TCAs are like a sledgehammer to the nervous system.Doctors know this. That’s why NICE guidelines in the UK and the Beers Criteria in the US both say: avoid TCAs in people over 65 unless every other option has failed. Yet they’re still prescribed. Why? Because they work - especially for nerve pain. But that benefit is shrinking as safer alternatives emerge. Duloxetine (Cymbalta) and venlafaxine (Effexor) are just as effective for pain and depression, with ACB scores of 0 or 1. No cognitive fog. No dry mouth. No memory slips.
The Cognitive Trap: Mistaking Drug Side Effects for Dementia
One of the most dangerous outcomes of high anticholinergic burden is misdiagnosis. Patients start forgetting names, losing keys, struggling to follow conversations. Their families assume it’s early dementia. Doctors order brain scans. They talk about Alzheimer’s. But what if it’s just the medicine? A 2022 study in Age and Ageing found that after stopping high-ACB drugs like TCAs, 63% of older adults showed measurable cognitive improvement within six months. Their MMSE scores - a standard test for dementia - went up by an average of 2.7 points. That’s not just a number. It’s someone remembering their grandchild’s birthday again. It’s someone driving safely without getting lost.Clinicians on Reddit’s psychiatry forum report the same thing: patients on amitriptyline for years, labeled as having mild cognitive impairment, then making a full recovery after switching to an SSRI. It’s not rare. It’s predictable. And it’s preventable.
Cardiac Risks: More Than Just an Irregular Beat
The heart doesn’t just respond to adrenaline. It runs on acetylcholine too. When TCAs block that signal, the heart loses its natural rhythm regulator. This leads to QT prolongation - a lengthening of the time between heartbeats. On an ECG, it looks like a stretched-out wave. In mild cases, it causes dizziness or palpitations. In severe cases, it can trigger torsades de pointes, a life-threatening arrhythmia that can kill within minutes.Amitriptyline is especially risky here. Studies show it can prolong the QRS complex - a measure of how fast electrical signals travel through the heart - by up to 50% in overdose. Even at normal doses, it increases the risk of arrhythmias by nearly three times compared to sertraline. That’s why cardiologists warn against TCAs in people with existing heart disease, high blood pressure, or a history of fainting. The therapeutic window is razor-thin: enough to help depression, but close to the edge of cardiac toxicity.
Who’s Most at Risk?
It’s not just the elderly. People over 50, especially those on multiple medications, are the highest risk group. But it’s also anyone taking over-the-counter antihistamines or sleep aids. A 2022 survey by the National Council on Aging found that 68% of older adults on TCAs reported at least two anticholinergic side effects - dry mouth, constipation, blurred vision, urinary retention, or memory problems. One in three said the cognitive issues were bad enough to consider quitting the drug.Women are often underdiagnosed here. They’re more likely to be prescribed TCAs for chronic pain or insomnia, and more likely to take OTC antihistamines for allergies. The cumulative burden hits harder. And because dementia is still wrongly seen as a “woman’s disease,” anticholinergic cognitive decline gets written off as aging - not drug-induced.

What Should You Do?
If you’re on a TCA, don’t panic. But do ask three questions:- What’s my total ACB score? (Add up all your meds - even OTC ones.)
- Have I been screened for cognitive changes in the last year?
- Have I been offered a safer alternative?
Deprescribing isn’t about quitting cold turkey. It’s about slow, supervised tapering. Nortriptyline is slightly less anticholinergic than amitriptyline, but both need a 4-8 week taper to avoid withdrawal. Switching to an SSRI like escitalopram or an SNRI like duloxetine often works better than expected. Cognitive symptoms often improve within weeks. Cardiac risks drop faster.
Ask your pharmacist or GP to run your full med list through an ACB calculator. Many UK and US electronic health systems now have this built in. If yours doesn’t, you can use the free online tool from bpacnz or the ACB Calculator from the University of Otago. Just plug in your pills - including NyQuil, Benadryl, or incontinence meds - and see your total score.
The Bigger Picture: Why This Matters Beyond One Drug
This isn’t just about TCAs. It’s about how we prescribe. We’ve normalized side effects like dry mouth and forgetfulness as “just part of getting older.” But they’re not. They’re signals. The rise of AI-powered prescribing tools that flag anticholinergic burden in real time - now being piloted in NHS trusts - shows we’re finally catching on. But change won’t come from technology alone. It comes from patients asking, “Could this be the medicine causing my memory problems?”TCAs still have a role - for treatment-resistant depression, for severe neuropathic pain when nothing else works. But they’re no longer first-line. They’re last-resort. And if you’re taking one, you deserve to know the full cost.
Can tricyclic antidepressants cause dementia?
They don’t cause dementia directly, but they significantly increase the risk of developing it. A seven-year study of over 3,400 adults over 65 found that long-term use of high-anticholinergic drugs, including TCAs, raised dementia risk by 54%. The cognitive decline from these drugs can mimic dementia and, in some cases, become permanent even after stopping the medication.
Is amitriptyline worse than other antidepressants for memory?
Yes. Amitriptyline has the highest possible anticholinergic burden score (ACB=3), meaning it strongly blocks acetylcholine - the brain chemical needed for memory and attention. SSRIs like sertraline and SNRIs like duloxetine have scores of 0 or 1, making them far less likely to affect cognition. Studies show patients switching from amitriptyline to these alternatives often regain memory function within months.
How do I know if my memory problems are from my medication?
If you started noticing memory lapses, confusion, or trouble concentrating after beginning a TCA or other anticholinergic drug, it’s likely related. The key sign is improvement after stopping - many patients report clearer thinking within weeks of tapering off. Ask your doctor to calculate your total Anticholinergic Cognitive Burden score. If it’s 3 or higher, your meds are likely contributing.
Are there safe alternatives to tricyclic antidepressants?
Yes. For depression, SSRIs like escitalopram or SNRIs like venlafaxine are first-line and have minimal anticholinergic effects. For chronic pain, duloxetine or pregabalin are effective alternatives. Non-drug options like cognitive behavioral therapy (CBT) or physical therapy also work well. Most patients respond just as well - or better - without the brain fog or heart risks.
Can I stop taking a TCA on my own?
No. Stopping TCAs suddenly can cause severe withdrawal - dizziness, nausea, anxiety, and even rebound depression. Always work with your doctor to taper slowly over 4-8 weeks. Your doctor may switch you to a safer antidepressant first, then gradually reduce the TCA to minimize discomfort.
Do over-the-counter drugs add to anticholinergic burden?
Absolutely. Common OTC sleep aids like diphenhydramine (Nytol, Benadryl) and allergy meds like chlorphenamine (Piriton) have ACB scores of 2 or 3. Even one of these can push your total burden into the danger zone. Many people don’t realize they’re adding to the risk because they think “it’s just a pill I buy at the store.”




George Hook
November 27, 2025 AT 19:09Let me tell you something that nobody talks about enough - this whole anticholinergic burden thing isn’t just a footnote in a pharmacology textbook. It’s a silent epidemic unfolding in living rooms across America, where grandmas are being told they’re ‘just getting forgetful’ while their medicine cabinet is slowly turning their brain to Swiss cheese. I’ve seen it in my own family. My uncle was on amitriptyline for ten years for sciatica, then started misplacing his keys, forgetting birthdays, and walking into walls. The doctor blamed age. I dug into his med list - benadryl for allergies, oxybutynin for bladder issues, and the TCA. ACB score? 9. He switched to duloxetine, tapered slowly, and within three months, he was back to telling jokes at Thanksgiving. Not a miracle. Just math. Toxic load minus exposure equals recovery. Why aren’t we screening this like blood pressure?
jaya sreeraagam
November 29, 2025 AT 04:44OMG I’m so glad someone finally said this!! I’ve been screaming about this for years but everyone thinks I’m crazy when I say ‘maybe it’s not dementia, maybe it’s your meds’ 😭 My mom was on nortriptyline + diphenhydramine + chlorpheniramine and she was forgetting her own phone number. We did the ACB calc - 8. She switched to sertraline + melatonin and now she remembers my kids’ names again. I cried. Like actual tears. Please, if you’re on any of these meds, talk to your pharmacist. They know more than your doctor sometimes. And yes, OTC means ‘over the counter’ not ‘over the edge of your brain’ 💪
Katrina Sofiya
November 30, 2025 AT 10:10As a clinical pharmacist with over two decades in geriatric care, I can say with absolute certainty that anticholinergic burden is one of the most underdiagnosed and preventable causes of cognitive decline in older adults. The literature is unequivocal: cumulative exposure to ACB ≥3 significantly increases dementia risk, and the damage is often irreversible. What’s more troubling is the normalization of polypharmacy - we prescribe for symptoms without considering systemic consequences. The Beers Criteria and STOPP/START guidelines exist for a reason. Yet, in practice, TCAs are still being initiated in patients over 65 without even a baseline MMSE. We need mandatory ACB scoring integrated into EHRs. Not optional. Mandatory. And we need to educate patients - not just providers. The power of asking ‘Could this be my medication?’ is revolutionary. It’s not resistance to treatment. It’s informed advocacy.
kaushik dutta
December 1, 2025 AT 15:31Let’s cut through the fluff. This isn’t about ‘risk’ - it’s about negligence. TCAs are 60-year-old technology. We have SSRIs, SNRIs, ketamine, TMS - all safer, all more targeted. Yet we keep prescribing amitriptyline like it’s the 1970s because it’s cheap and doctors are lazy. And don’t get me started on the OTC anticholinergics. People pop Benadryl like candy because ‘it helps me sleep.’ Guess what? It’s not helping you sleep - it’s poisoning your cholinergic system. This isn’t ‘side effect’ - it’s iatrogenic dementia. The fact that this is still happening in 2025 is a moral failure. If your doctor won’t de-prescribe, find a new one. Your brain isn’t disposable.
doug schlenker
December 2, 2025 AT 06:36I appreciate the depth of this post - really, I do. I’ve been on nortriptyline for chronic migraines for six years. I didn’t realize my ‘brain fog’ was from the med until I read this. I’ve been feeling off for ages - forgetful, sluggish, like my thoughts were underwater. I didn’t connect it to the pill. I thought it was stress. But now I’m going to ask my doctor about switching. I’m scared to stop, though. What if it makes my headaches worse? I just need to know - if I switch to duloxetine, will the fog lift fast? Or is it a slow climb back?
Olivia Gracelynn Starsmith
December 3, 2025 AT 06:47Just wanted to say thank you for writing this. I’m a nurse and I’ve seen so many elderly patients get labeled with dementia only to improve dramatically after deprescribing. One woman, 78, was in a memory care unit because she couldn’t remember her daughter’s name. She was on amitriptyline, diphenhydramine, and oxybutynin. ACB score 9. We tapered slowly, switched to gabapentin and citalopram. Three months later - she was laughing, knitting, calling her daughter by name. No scan. No meds. Just removing the poison. This isn’t theoretical. It’s real. And it’s happening every day. Please share this with your parents. Or your grandparents. Or your doctor.
Skye Hamilton
December 3, 2025 AT 08:11Okay but… what if I just like the dry mouth? I mean, it’s kind of nice? Like, I don’t want to be ‘with it’ all the time. Sometimes I like being a little spaced out. And honestly, I don’t care if I forget where I put my keys. My keys are overrated. Also, I think dementia is just capitalism’s way of making old people feel guilty for existing. Why fight it? Just… chill. Maybe the meds are helping me be more zen.
Maria Romina Aguilar
December 4, 2025 AT 03:15Are you… sure… about this…? I mean… I’ve read… some… papers… that say… the correlation… might… be… confounded… by… comorbidities…? And… what about… the… placebo… effect… in… cognitive… improvement…? And… isn’t… it… possible… that… people… who… stop… TCAs… are… just… more… health-conscious…? So… maybe… it’s… not… the… drug…? Maybe… it’s… the… lifestyle… change…? Just… saying…
Brandon Trevino
December 5, 2025 AT 07:22Let us not confuse pharmacological mechanisms with clinical outcomes. The ACB scale, while useful as a heuristic, is a crude proxy. It assigns equal weight to a 25mg dose of diphenhydramine and a 100mg dose of nortriptyline - ignoring pharmacokinetics, receptor affinity, and individual metabolic variance. The 54% increased dementia risk cited? Derived from observational studies with residual confounding. The real issue is polypharmacy - not any single agent. Moreover, TCAs remain indispensable for treatment-resistant depression and neuropathic pain in patients who fail all other modalities. To demonize them is not evidence-based medicine - it is dogma masquerading as advocacy. We must individualize care, not generalize fear. A 70-year-old with refractory fibromyalgia and no cardiac history may derive more benefit than harm. The risk-benefit calculus is not binary. It is nuanced. And it requires clinical judgment - not algorithmic reductionism.
Denise Wiley
December 6, 2025 AT 23:24THIS. THIS. THIS. I’m a 58-year-old woman who was on amitriptyline for 8 years for fibro and insomnia. I thought I was just ‘getting old.’ I forgot my wedding anniversary. I cried for no reason. I couldn’t follow TV plots. My husband said I was ‘not myself.’ Then I found this ACB calculator. Score: 8. I switched to venlafaxine. Within 6 weeks - I remembered my mom’s phone number. I started reading again. I danced in the kitchen. I didn’t know I’d lost so much until I got it back. Please, if you’re on a TCA - don’t wait. Talk to your doctor. Ask for the score. You’re not ‘crazy.’ You’re just medicated. And you deserve better.
Hannah Magera
December 7, 2025 AT 14:24So if I take one TCA and one allergy pill, that’s bad? Like… how bad? Should I be scared? I don’t know what ACB means. Can someone just tell me - should I stop my meds? Or just stop the Benadryl? I’m confused.