If you or someone you care about uses an inhaler for asthma or COPD, here’s the hard truth: you’re probably not using it right. Studies show 70 to 90% of people get the technique wrong. That means most of the medicine never reaches the lungs. Instead, it lands in your mouth, throat, or even on the floor. You’re paying for medication that isn’t working - and your symptoms keep getting worse.
Why Technique Matters More Than the Device
There are dozens of inhalers on the market: metered-dose inhalers (MDIs), dry powder inhalers (DPIs), and soft mist inhalers like Respimat. Each looks different. Each feels different. But here’s what no one tells you: the device doesn’t matter as much as how you use it.A 2023 review by the Agency for Healthcare Research and Quality found that when used correctly, all inhalers work about the same. But in real life, improper technique cuts effectiveness by 30 to 40%. That’s like taking half a dose every time. You might think your medicine isn’t strong enough. It’s not. You’re just not getting it where it needs to go.
Dr. Robert Openbush from the American Lung Association says it plainly: “Proper technique is the single most important factor in inhaler effectiveness, more critical than the specific device chosen.”
How MDIs Work - And Why Most People Fail
Metered-dose inhalers (MDIs) are the most common. Think of them like tiny spray cans: press down while you breathe in. Sounds simple, right? It’s not.Most people press the canister too early - before they start inhaling. Or they press it too late - after they’ve already breathed in. Either way, the medicine shoots into the back of the throat. That’s why so many people get a sore throat or oral thrush. The steroid in the inhaler sticks to the mucous membranes, not the lungs.
The correct method for an MDI is a 7-step process:
- Remove the cap and shake the inhaler well (4-5 shakes).
- Exhale fully - away from the inhaler.
- Place the mouthpiece in your mouth, sealing your lips around it.
- Start breathing in slowly through your mouth, and press the canister at the same time.
- Keep inhaling slowly for 3 to 5 seconds.
- Hold your breath for 10 seconds. This lets the medicine settle in your airways.
- Exhale slowly through your nose.
And here’s the kicker: wait a full 60 seconds between puffs. If you rush, the second puff won’t reach deep into your lungs. Most people don’t know this.
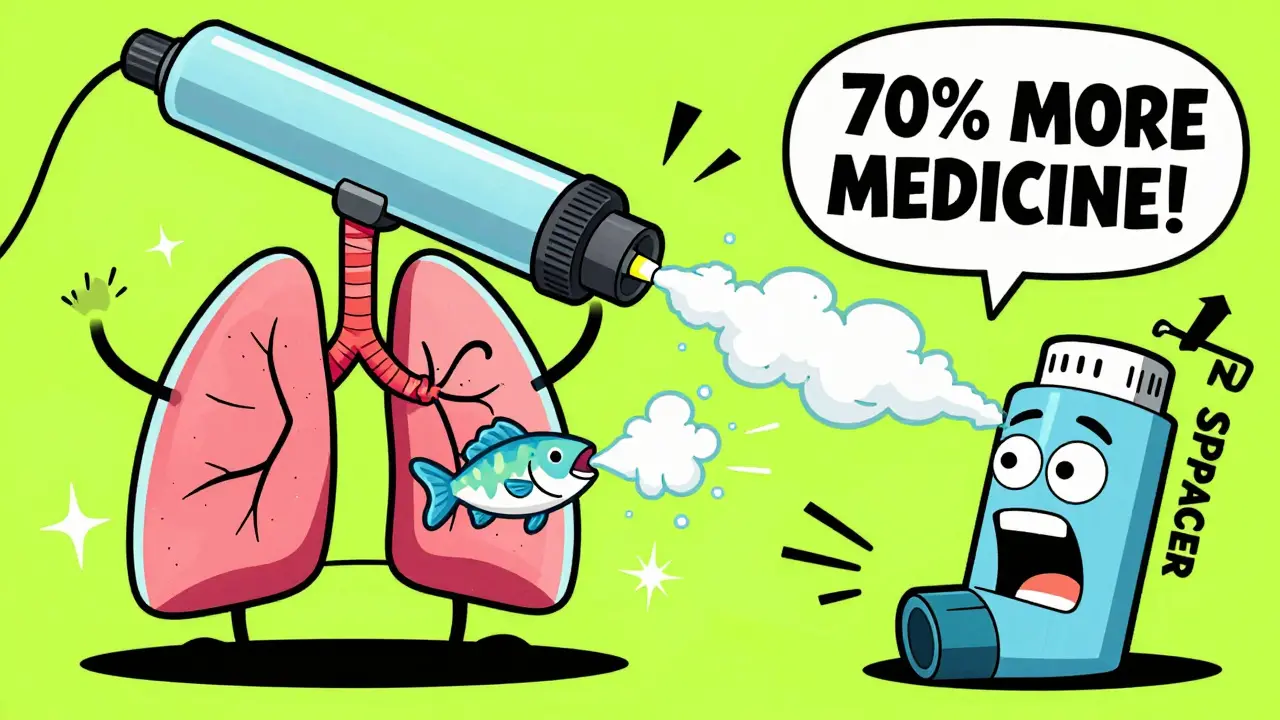
Spacers: The Secret Weapon You’re Not Using
If you’re using an MDI without a spacer, you’re making things harder on yourself. A spacer is a plastic tube that attaches to the inhaler. It holds the medicine in a chamber while you breathe in slowly.Studies show spacers increase lung delivery by 70 to 100%. That’s not a small improvement - it’s the difference between barely helping and actually controlling your symptoms. The Global Initiative for Asthma (GINA) recommends spacers for every MDI user, no exceptions.
Spacers are especially helpful for children, older adults, and anyone who struggles with timing. They eliminate the need for perfect hand-breath coordination. You just press the inhaler, then breathe in normally through the spacer for 5 seconds. Hold for 10. Done.
And yes - spacers are cheap. Most pharmacies sell them for under $15. Insurance often covers them. If your doctor didn’t give you one, ask. Don’t assume you don’t need it.
Dry Powder Inhalers: Faster, But Only If You Can Breathe Hard Enough
Dry powder inhalers (DPIs) like Diskus, Turbuhaler, and Ellipta don’t need a propellant. You breathe in fast and hard to pull the powder into your lungs. That sounds great - until you realize how much force you actually need.DPIs require an inspiratory flow of 60 to 90 liters per minute. That’s like taking a deep, sudden breath through a straw. If you have severe COPD, your lungs might not be strong enough to generate that airflow. In fact, a 2021 study in the European Respiratory Journal found that nearly half of patients with advanced COPD couldn’t use DPIs effectively.
And here’s another problem: if you breathe too slowly, the powder won’t aerosolize. It just sits in your mouth. That’s why so many users report coughing fits or a gritty feeling in their throat. Thirty-one percent of COPD patients surveyed by the COPD Foundation said they had this issue.
Important: Never use a spacer with a DPI. It blocks the airflow and cuts medication delivery by 50 to 70%. That’s not a mistake - it’s a rule. If you’re using a spacer with your Diskus or Turbuhaler, stop. You’re wasting your medicine.
Soft Mist Inhalers: The Middle Ground
Soft mist inhalers like Respimat are newer. They don’t need a strong breath. Instead, they release a slow, gentle mist over 1.5 seconds. You just breathe in normally.They’re a good option for people who can’t manage the fast inhalation of DPIs or the timing of MDIs. But they’re not magic. You still need to:
- Prime the device before first use (follow the instructions - it’s different for every model).
- Exhale before inhaling.
- Hold your breath for 10 seconds after.
And you still need to rinse your mouth after using corticosteroids. Same rule applies.
The Biggest Mistakes (And How to Fix Them)
Here’s what most people do wrong - and how to fix it:- Not shaking the inhaler - 45% of users skip this. Shake it 4-5 times before each puff. Even if it’s new.
- Exhaling into the device - 27% do this. Always exhale away from the inhaler. Moisture inside ruins the medicine.
- Not holding breath - 63% don’t hold for 10 seconds. That’s the most common error. Hold it. Count to 10. Let the medicine settle.
- Removing DPI capsules - 15% try to open the capsule. Don’t. The device is designed to pierce it automatically.
- Storing inhalers in hot places - If your inhaler sits in a car or bathroom, the medicine loses 15-20% of its potency. Keep it at room temperature (20-25°C).
When to Rinse Your Mouth - And Why
If your inhaler contains a corticosteroid (like fluticasone, budesonide, or mometasone), rinse your mouth with water after every use. Swish and spit. Don’t swallow.Why? Steroids can cause oral thrush - a fungal infection that looks like white patches in your mouth. It’s painful and can make swallowing hard. A 2022 study in the Chest Journal found rinsing reduces thrush risk by 75%. It’s that simple.
Even if you feel fine, do it. Prevention beats treatment every time.

What About Smart Inhalers?
There’s new tech out there. Smart inhalers like Propeller Health attach a tiny sensor to your device. It tracks when you use it, how hard you inhale, and even reminds you if you miss a dose. A 2022 study in Annals of Internal Medicine found these sensors detect technique errors with 92% accuracy.They’re not a magic fix - but they’re a game-changer for people who forget doses or don’t know if they’re using it right. The FDA approved the first one in 2021. By 2025, 40% of inhalers are expected to have digital tracking.
They’re expensive, and insurance doesn’t always cover them. But if you’re still struggling after multiple doctor visits, it might be worth asking about.
What Your Doctor Should Be Doing - And Isn’t
The National Asthma Education and Prevention Program says doctors should check your inhaler technique at every visit. But most don’t. A 2023 study in JAMA Internal Medicine found that when doctors did check technique, patients had 22% fewer emergency visits.Don’t wait for your doctor to ask. Bring your inhaler to every appointment. Say: “Can you watch me use this?” Then do it slowly. Let them see your technique. If they don’t watch, ask again. This is your health.
In countries like the UK, where there are national training programs (“Inhaler Champions”), 75% of patients use their inhalers correctly. In places without training, it’s only 45%. You can’t rely on luck. You need to learn - and relearn - properly.
Final Advice: Practice, Don’t Assume
You’ve probably been using your inhaler for months or years. But that doesn’t mean you’re doing it right. Technique isn’t something you learn once. It’s something you practice.Watch a video from the American Lung Association or the Global Initiative for Asthma. Do it in front of a mirror. Feel the spray. Notice where it lands. Try it with a spacer. Try it without. See the difference.
And if you’re still not sure? Go back to your pharmacist. They’re trained to show you how to use inhalers. Most will do it for free. No appointment needed.
Your inhaler isn’t broken. You’re just not using it right. Fix the technique, and you might find your symptoms improve - without changing your medicine, without higher doses, without more pills. Just by breathing better.
Can I use my inhaler without shaking it?
No. Shaking your inhaler for 4-5 seconds before each puff ensures the medication and propellant are properly mixed. Skipping this step means you might get a weak or uneven dose - sometimes no medicine at all. Always shake it.
Why does my inhaler make me cough?
Coughing after using an inhaler usually means the medicine isn’t reaching your lungs. With MDIs, it’s often because you didn’t coordinate pressing and breathing. With DPIs, it’s because you didn’t inhale fast or hard enough. The powder gets stuck in your throat. Try using a spacer with an MDI, or practice deeper breaths with a DPI. If it keeps happening, ask your doctor to check your technique.
Is it okay to use two different inhalers at the same time?
Only if your doctor specifically told you to. Using multiple inhalers without training increases the risk of mixing up techniques. The European Respiratory Society says technique confusion can reduce effectiveness by 35-50%. Stick to one type per category (e.g., one rescue inhaler, one maintenance inhaler) unless you’ve been trained on both.
Do I need a spacer with my DPI?
No. Spacers are only for metered-dose inhalers (MDIs). Using a spacer with a dry powder inhaler (DPI) blocks the airflow needed to release the powder. This cuts your medication delivery by 50-70%. Never use a spacer with a Diskus, Turbuhaler, or Ellipta.
How long should I hold my breath after using an inhaler?
Hold your breath for 10 seconds after inhaling. This gives the medicine time to settle in your airways instead of being exhaled right away. Studies show this increases lung deposition by 20-30%. If you can’t hold for 10 seconds, do as long as you can - even 5 seconds helps more than nothing.
Can I store my inhaler in the bathroom?
No. Heat and humidity damage the medication. Bathrooms are too warm and moist. Store your inhaler at room temperature (20-25°C), like in a bedroom drawer. If it’s been left in a hot car or near a heater, the dose may be less effective. Replace it if you’re unsure.
What if my inhaler runs out but still makes a sound?
Many inhalers make a clicking sound even after the medicine is gone. That doesn’t mean it still works. Always check the counter on your inhaler - most have one. If it says “0” or “empty,” stop using it. Using an empty inhaler during an attack can be dangerous. Keep a spare on hand.



Ajay Sangani
December 22, 2025 AT 18:25still breathing though, i guess?
Katie Taylor
December 24, 2025 AT 12:47Wilton Holliday
December 24, 2025 AT 23:09Spacers are a game-changer. Mine cost $12 at CVS. My kid uses one too - no more thrush.
Pro tip: Practice in front of a mirror with water. You’ll see exactly where the mist goes. It’s wild how much difference it makes. You got this.
Abby Polhill
December 26, 2025 AT 18:56Spacers mitigate oropharyngeal deposition by 70-100%, per GINA 2023 guidelines. However, their use with DPIs induces laminar flow disruption, reducing aerosolization efficiency by 50-70%.
Smart inhalers with IoT telemetry (e.g., Propeller) demonstrate 92% accuracy in technique error detection, yet cost and reimbursement remain barriers to scalability.
Bret Freeman
December 28, 2025 AT 11:20You’re telling me millions of people are wasting hundreds of dollars a year on medicine that’s landing in their throat? And no one’s held them accountable?
This is medical negligence. Someone should sue every pharmacy that doesn’t offer a free technique demo. I’m starting a petition.
Austin LeBlanc
December 29, 2025 AT 00:56Some of us have our own routines. You think your way is the only way? I shake it twice, not four times. I hold my breath for 5 seconds. It works for me.
Stop shaming people. Not everyone needs a 7-step manual.
Rachel Cericola
December 29, 2025 AT 18:31Here’s the truth: technique is 80% of the battle. The device? Only 20%.
Most people don’t realize you need to exhale AWAY from the inhaler - not into it. Moisture ruins the dose. I’ve seen people store theirs in the bathroom. That’s like keeping your insulin in a sauna.
And if you’re using a corticosteroid inhaler and not rinsing? You’re asking for thrush. It’s not a myth. I’ve seen it. It’s painful. It’s preventable.
Bring your inhaler to your next appointment. Say, ‘Watch me.’ If they don’t, ask again. Your lungs are worth it.
Blow Job
December 30, 2025 AT 20:00My doctor didn’t even ask about technique until I showed him the data. Now I use a spacer, rinse every time, and keep my inhaler in my bedside drawer - not the bathroom.
It’s not about being perfect. It’s about being aware. You’re not broken. You just didn’t know. Now you do.
Christine Détraz
December 30, 2025 AT 20:18She’s had one coughing fit since. Not one.
It’s not about being a medical expert. It’s about being willing to learn. Even at 78.
John Pearce CP
January 1, 2026 AT 19:28Compare this to the United Kingdom, where the Inhaler Champion program has increased correct usage to 75%. Why? Because they mandate technique verification at every visit.
We do not. We treat inhalers like over-the-counter painkillers. This is not acceptable.
It is time for federal regulation. Mandatory training. Certification for prescribers. This is not a suggestion. It is a moral imperative.
EMMANUEL EMEKAOGBOR
January 2, 2026 AT 23:09But I’ve also seen community health workers in Lagos teach proper technique with just a mirror and a bottle of water. No fancy gadgets. Just patience.
It’s not about money. It’s about care. This post reminds me that even in places with few resources, knowledge can still be shared - and lives can still be saved.
CHETAN MANDLECHA
January 3, 2026 AT 09:20Don’t wait for the system. Make it work. Your lungs don’t care if it’s fancy.
Pankaj Chaudhary IPS
January 3, 2026 AT 09:36I’ve trained over 300 patients in Delhi using this exact method. Every single one improved. Not because their meds changed. Because their technique did.
If you’re reading this - you’re one step ahead. Now go show someone else how to breathe right.