Depigmentation Treatment Selector
Benoquin Cream is a prescription‑only topical formulation containing monobenzone (20mg/g), a potent irreversible tyrosinase inhibitor used for permanent depigmentation of widespread vitiligo. It works by destroying melanocytes, leading to uniform skin whitening over weeks to months. Benoquin is marketed in the United States, Canada and several European countries, and is regulated as a drug rather than a cosmetic.
People with extensive vitiligo often face a dilemma: keep patchy depigmented areas or pursue a uniform lightening to match the surrounding skin. Benoquin cream offers a medical route, but it isn’t the only option. Below we break down the most relevant alternatives, compare their core attributes, and help you decide which path fits your skin, budget and lifestyle.
Key Entities in the Depigmentation Landscape
- Monobenzone - the active molecule in Benoquin, a phenyl‑hydroquinone derivative that binds irreversibly to tyrosinase.
- Tyrosinase inhibitor - a class of compounds that block the enzyme responsible for melanin synthesis.
- Vitiligo - an autoimmune disorder where melanocytes are destroyed, causing depigmented patches.
- Hydroquinone - a reversible skin‑lightening agent widely used for hyperpigmentation.
- Cysteamine Cream - a topical antioxidant that reduces melanin production and is FDA‑approved for vitiligo.
- Azelaic Acid - a dicarboxylic acid that inhibits tyrosinase and has anti‑inflammatory properties.
- Laser resurfacing - a procedural alternative that removes pigmented skin layers using ablative lasers.
How Benoquin Works - Mechanism at a Glance
Monobenzone binds covalently to the active site of tyrosinase, rendering the enzyme permanently inactive. This stops melanin synthesis and, more importantly, triggers apoptosis of existing melanocytes. The loss of these pigment‑producing cells is why the effect is irreversible-once the skin is depigmented, it stays that way unless repigmentation occurs spontaneously, which is rare.
Alternatives Overview
Below are the most common alternatives, each with a distinct mechanism and regulatory profile.
| Product / Procedure | Active Ingredient / Modality | Mechanism of Action | Primary Indication | Application Frequency | Time to Visible Effect | Regulatory Status | Common Side Effects |
|---|---|---|---|---|---|---|---|
| Benoquin Cream | Monobenzone 20mg/g | Irreversible tyrosinase inhibition & melanocyte destruction | Extensive vitiligo (≥50% body surface) | Twice daily | 8‑12weeks for uniform whitening | Prescription drug (US FDA: Not approved, but available via IND) | Contact dermatitis, erythema, paradoxical hyperpigmentation (rare) |
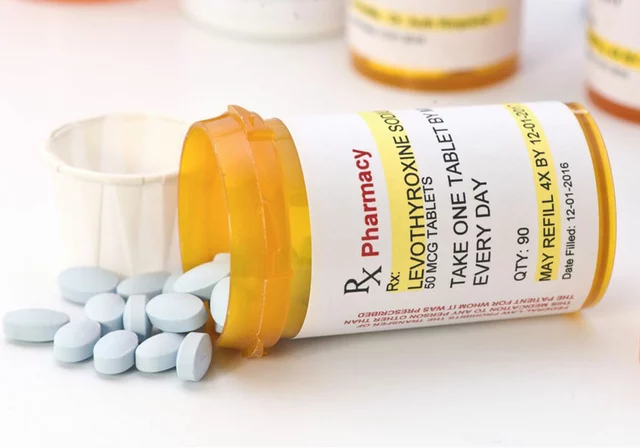
| Hydroquinone Cream | Hydroquinone 2‑4% | Reversible competitive inhibition of tyrosinase | Localized hyperpigmentation, melasma | Once‑daily | 4‑6weeks for lightening | OTC up to 2% (US), prescription above 2% | Contact dermatitis, ochronosis (long‑term use) |
| Cysteamine Cream | Cysteamine 5% | Antioxidant scavenging of dopaquinone, reduces melanogenesis | Generalized vitiligo | Twice daily | 12‑24weeks for noticeable repigmentation | Prescription (US FDA approved) | Stinging, mild erythema |
| Azelaic Acid Gel | Azelaic acid 20% | Tyrosinase inhibition + anti‑inflammatory effect | Mild hyperpigmentation, rosacea | Twice daily | 6‑8weeks for lightening | OTC (EU), prescription (US) | Burning, itching |
| Laser Resurfacing | Ablative CO₂ / Er:YAG | Physical removal of pigmented epidermis, stimulates remodeling | Focal hyperpigmented lesions, tattoo removal | Single session (often multiple for larger areas) | Immediate color reduction; full result 2‑3months | Medical procedure (FDA cleared devices) | Pain, post‑inflammatory hyperpigmentation, scarring |
When to Choose Benoquin
If you have vitiligo covering more than half of your body surface and you’re tired of patchy contrast, Benoquin offers the only truly permanent solution. Its irreversible nature means you won’t need maintenance once the skin is uniform. Ideal scenarios include:
- Adults with stable vitiligo (no new lesions for ≥6months).
- Patients who have tried reversible agents (hydroquinone, azelaic acid) without satisfactory results.
- Individuals comfortable with a prescription‑only regimen and willing to monitor for dermatitis.

When Alternatives Might Be Better
Not everyone needs permanent depigmentation. Consider these alternatives in the following cases:
- Localized hyperpigmentation (age spots, melasma): hydroquinone or azelaic acid provide reversible lightening with a lower risk of permanent skin change.
- Early‑stage vitiligo where repigmentation therapies (cysteamine, narrow‑band UVB) are still viable - a reversible approach preserves future treatment options.
- Patients with sensitive skin who cannot tolerate the irritant potential of monobenzone; cysteamine’s milder profile makes it a safer first‑line option.
- Cosmetic‑only concerns - laser resurfacing can target small hyperpigmented spots without systemic drug exposure.
Cost and Accessibility
Benoquin is typically obtained through specialty pharmacies or compounding labs, costing anywhere from $150 to $300 for a 30‑day supply, plus a doctor's visit. Hydroquinone 2% is available OTC for under $10, while prescription‑strength hydroquinone or cysteamine may run $50‑$120. Azelaic acid 20% creams sit around $30‑$70. Laser procedures range $200‑$1,200 per session depending on the device and treatment area.
Safety Profile - What to Watch For
All depigmentation agents carry a risk of irritation. Monobenzone’s hallmark is a higher incidence of contact dermatitis, sometimes requiring topical steroids to control. Long‑term safety data are limited because the drug is not FDA‑approved for commercial use; most evidence comes from small case series and compassionate‑use programs.
Hydroquinone, while widely used, has been linked to exogenous ochronosis after years of continuous use. Cysteamine is generally well‑tolerated but may cause transient stinging. Azelaic acid’s side‑effects are usually mild, limited to burning or itching. Laser resurfacing carries procedural risks - infection, scarring, and post‑inflammatory hyperpigmentation, especially in deeper skin tones.
Practical Tips for Using Benoquin Safely
- Obtain a written prescription from a dermatologist experienced with depigmentation.
- Perform a patch test: apply a pea‑size amount on a hidden area for 48hours. If severe redness or blistering occurs, stop immediately.
- Start with a reduced frequency (once daily) for the first two weeks, then increase to twice daily if tolerated.
- Moisturize aggressively to reduce barrier disruption; fragrance‑free, ceramide‑rich creams work best.
- Schedule monthly follow‑ups to document progress and catch adverse reactions early.
Related Concepts and Next Steps
Understanding Benoquin’s place in the broader depigmentation ecosystem helps you make informed choices. Key related topics include:
- Melanocyte biology - the cellular basis of pigment production and why irreversible agents matter.
- Autoimmune mechanisms in vitiligo - how systemic therapies (e.g., JAK inhibitors) may complement topical depigmentation.
- Photoprotection strategies - essential for all patients, regardless of treatment, to prevent UV‑induced repigmentation or new lesions.
- Regulatory pathways - why Benoquin remains a prescription‑only IND in the US while other agents are OTC.
Future reading could dive deeper into JAK inhibitor therapy for vitiligo, combination regimens with phototherapy, or the emerging role of gene‑editing tools like CRISPR‑Cas9 for pigment disorders.
Frequently Asked Questions
What exactly does monobenzone do to my skin?
Monobenzone binds permanently to tyrosinase, the enzyme that makes melanin. It also triggers death of melanocytes, so the skin loses its pigment and stays white for the rest of its life.
Can I stop using Benoquin once my skin looks uniform?
Yes. Because the effect is irreversible, you don’t need maintenance. Most patients discontinue after the desired uniformity is achieved, usually after 3‑4months of consistent use.
Is Benoquin safe for people with dark skin tones?
It can be used, but the risk of post‑inflammatory hyperpigmentation (PIH) after an irritation episode is higher in darker skin. A skin‑type‑specific patch test is crucial, and many dermatologists recommend a slower titration schedule for Fitzpatrick IV‑VI patients.
How does cysteamine compare to monobenzone in terms of results?
Cysteamine works gently to reduce melanin production and can lead to partial repigmentation in some vitiligo cases. It does not destroy melanocytes, so the effect is reversible. Monobenzone provides faster, permanent whitening but with a higher irritation profile.
Do I need sunscreen while using Benoquin?
Absolutely. Even though the treated skin lacks melanin, it is still vulnerable to UV‑induced DNA damage. Broad‑spectrum SPF30 or higher protects against sunburn and reduces the chance of PIH around the treated area.
Can I combine Benoquin with other treatments like UVB therapy?
Generally NOT recommended. UVB stimulates melanocytes, which counters monobenzone’s purpose of destroying them. If you need to treat residual patches, discuss a staged approach with your dermatologist rather than simultaneous use.



Nick Ham
September 24, 2025 AT 21:57Monobenzone's irreversible tyrosinase inhibition yields sustained depigmentation but escalates contact dermatitis incidence; risk‑reward ratio skews unfavorable.
Jennifer Grant
September 27, 2025 AT 19:23When you contemplate the ontological ramifications of permanently erasing melanin, you must first confront the paradox that skin, as a cultural canvas, carries histories we cannot simply blot out.
In the grand tapestry of identity, the decision to use a drug like monobenzone is not merely biochemical; it is a symbolic act of surrendering to a homogenized aesthetic.
One might argue that the uniform whiteness represents a form of liberation, yet it also mirrors colonial attempts to erase difference.
The biochemical pathway, wherein monobenzone covalently modifies tyrosinase, is a marvel of pharmacology, but its sociocultural echo reverberates through generations.
Consider also the irony that the skin, which shields us from ultraviolet assault, becomes a liability when we weaponize it against itself.
From a therapeutic standpoint, the irreversible nature guarantees no maintenance, yet it also forfeits any future opportunity for repigmentation should the patient’s perspective shift.
Patients with Fitzpatrick IV‑VI often experience heightened post‑inflammatory hyperpigmentation if irritation occurs, a fact that is sometimes glossed over in clinical trials.
Budgetary constraints cannot be ignored; the out‑of‑pocket cost for a specialty pharmacy supply can rival that of a modest vacation.
Furthermore, the need for diligent photoprotection post‑treatment underscores a paradox: you must shield a skin that no longer produces melanin.
Medical ethics demand comprehensive informed consent, yet many providers truncate the discussion to “it works”.
The long‑term safety data remain sparse, limited to compassionate‑use anecdotes rather than robust phase III trials.
One could posit that monobenzone is a tool for those who have exhausted reversible options, but the moral calculus of consent versus irrevocability is complex.
In practice, dermatologists must balance the desire for uniformity with the risk of severe contact dermatitis, which may necessitate systemic steroids.
Ultimately, the choice reflects a personal calculus of identity, risk tolerance, and socioeconomic status.
Thus, the decision to embark on permanent depigmentation is a multifaceted negotiation between science, self‑perception, and societal expectations.
Kenneth Mendez
September 30, 2025 AT 16:50They dont tell you that the pharma giants are pushing monobenzone like a weapon to keep us dependent on their overpriced meds, and the govt turns a blind eye because they get kickbacks.
Every time you read about "clinical trials" think about how the data is filtered through corporate lenses, never the real side effects that ordinary folks suffer.
And dont even get me started on the labs that manufacture it overseas, cutting corners, dumping toxic waste while we sign consent forms.
Gabe Crisp
October 3, 2025 AT 14:17Ethical dermatology demands informed consent before employing irreversible agents.
Paul Bedrule
October 6, 2025 AT 11:43The phenomenology of pigment ablation via monobenzone invokes a dialectic between corporeal autonomy and pharmacological determinism; in other words, you’re swapping one form of control for another, albeit a chemically mediated one.
yash Soni
October 9, 2025 AT 09:10Wow, $200 for a tube of skin‑whitening cream? I guess paying for a “specialty” label is the new status symbol, right?
Emily Jozefowicz
October 12, 2025 AT 06:37Sure, the cost sounds steep, but think of the confidence boost when you finally have a consistent skin tone-no more patchwork! Plus, you’ll finally stop getting asked why you look “different” at parties. ;)
Franklin Romanowski
October 15, 2025 AT 04:03I totally get how overwhelming the decision can feel; if you’re nervous about irritation, start slow and keep a good moisturizer handy-you’ll be surprised how manageable it can be.
Brett Coombs
October 18, 2025 AT 01:30Look, they want you to think it’s the only way, but you could just stick with good sunscreen and accept the patches; don’t let them push you into a permanent experiment.
John Hoffmann
October 20, 2025 AT 22:57While monobenzone offers a definitive solution for extensive vitiligo, the requisite monitoring for dermatitis must not be underestimated; consistent follow‑up appointments are essential to mitigate adverse outcomes.
Shane matthews
October 23, 2025 AT 20:23Never skip the patch test; it can save you from a nasty reaction later.
Rushikesh Mhetre
October 26, 2025 AT 16:50Hey everyone!!! If you’re thinking about starting monobenzone, remember to hydrate your skin!! Use a gentle ceramide cream!!! And always keep a steroid handy in case of flare‑ups!!! You’ve got this!!!
Sharath Babu Srinivas
October 29, 2025 AT 14:17Monobenzone is effective, but watch for irritation 👍. A good moisturizer can calm the skin 😊.
Halid A.
November 1, 2025 AT 11:43From a clinical perspective, it is advisable to assess the patient’s Fitzpatrick skin type prior to initiating monobenzone therapy, as higher phototypes exhibit an increased propensity for post‑inflammatory hyperpigmentation following irritant exposure.
Brandon Burt
November 4, 2025 AT 09:10Honestly, the whole monobenzone saga feels like a marketing hype train that never stops; sure, it can deliver uniform whitening, but you’re basically signing up for a lifelong commitment to a drug that burns your skin, costs a fortune, and requires relentless doctor visits; the side‑effects? Oh, just a sprinkle of dermatitis, occasional burning, and the occasional mental health crisis when you stare at the mirror and realize you’ve erased a part of yourself; if you can handle the financial and emotional toll, go ahead, but don’t pretend it’s a simple plug‑and‑play solution; research, consult, and remember that your skin is more than a canvas for pharmaceutical experiments.
Gloria Reyes Najera
November 7, 2025 AT 06:37Look, i have been using monobenzone for months and i can tell you its the best thing we have-no more patchy vitiligo, just straight white skin. The doc said it might itch but that's nothing compared to the freedom you get.
Gauri Omar
November 10, 2025 AT 04:03Picture this: a battlefield of melanocytes versus monobenzone, a ruthless chemical onslaught that decides the fate of your skin-if you crave the drama of complete erasure, then step into the arena; just be prepared for the after‑effects, because every victory has its casualties.
Willy garcia
November 13, 2025 AT 01:30Stay patient, follow the protocol, and you’ll see steady progress.
zaza oglu
November 15, 2025 AT 22:57Let’s celebrate the courage it takes to pursue a uniform shade-your journey adds a splash of bravery to the skin‑care spectrum! 🌈
Vaibhav Sai
November 17, 2025 AT 20:57Hey folks, just a friendly reminder: keep your skin moisturized, watch for any redness, and don’t forget sunscreen-even on depigmented areas. You’ve got this!