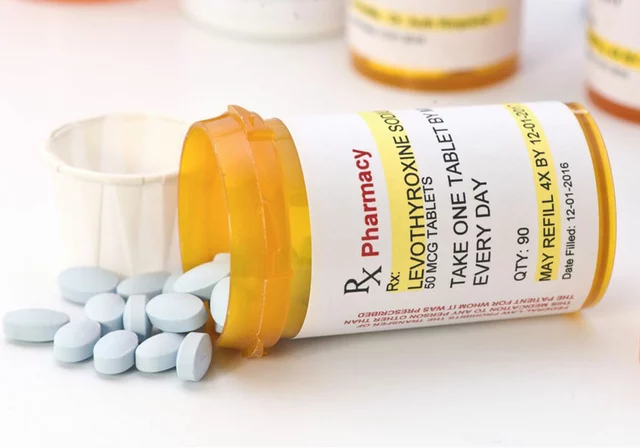
For decades, Medicare couldn’t negotiate drug prices. That changed in 2022 when the Inflation Reduction Act gave Medicare the power to directly talk to drugmakers and set fair prices for the most expensive medications. Starting January 1, 2026, this new system kicks in for 10 top-selling drugs - and the discounts are huge. Some are dropping by more than 70%. This isn’t just a policy change. It’s a shift in how millions of Americans pay for their prescriptions.
What exactly is being negotiated?
The Medicare Drug Price Negotiation Program targets drugs that are expensive, have no generic or biosimilar alternatives, and have been on the market for at least seven years (or 11 for biologics). These aren’t new wonder drugs - they’re the ones that have dominated sales for years. The first 10 include Eliquis (for blood clots), Jardiance (for diabetes), and Xarelto (another blood thinner). Together, these drugs cost Medicare $50.5 billion in 2022. Eliquis alone accounted for $6.3 billion.
Before this law, Medicare paid whatever drugmakers charged. Private insurers could negotiate rebates behind the scenes, but Medicare was locked out. Now, the Centers for Medicare & Medicaid Services (CMS) sets a Maximum Fair Price - the highest amount Medicare will pay. This price is based on what the drug costs in other countries, how much it’s used, what alternatives exist, and what manufacturers actually get paid after rebates and discounts.
How the negotiation process actually works
It’s not a back-and-forth haggle at a car dealership. It’s a tightly timed, rule-bound process with strict deadlines. On February 1, 2024, CMS sent each drugmaker an initial offer. They had 30 days to respond with a counteroffer. Then, CMS met with each company - three times - between March and August 2024. Five deals were settled in those meetings. The other five were finalized through written offers.
The final price can’t be higher than two limits: either the weighted average of what private insurers paid (after all rebates), or a percentage of the drug’s average price in the U.S. market. CMS didn’t just guess - they used real data from pharmacy claims, manufacturer reports, and clinical studies. For example, if a drug has cheaper alternatives that work just as well, CMS uses that to push the price down.
By August 1, 2024, all 10 negotiations were complete. The discounts ranged from 38% to 79%. That means if a 30-day supply of Eliquis used to cost $500, it might now cost $120 under Medicare’s new price.
Who benefits - and how?
The biggest winners are Medicare beneficiaries, especially those stuck in the coverage gap - the "donut hole."
Before, people paid 25% of the full price even after rebates. Now, with the negotiated price, that 25% is based on a much lower number. Someone taking Jardiance might go from paying $150 a month out-of-pocket to $40. That’s life-changing for seniors on fixed incomes.
Medicare itself saves billions. The Congressional Budget Office estimates $98.5 billion in savings over 10 years. That money doesn’t vanish - it helps lower premiums for everyone in Part D and reduces pressure on the federal budget.
But here’s the catch: private insurers might also benefit. When Medicare sets a new price, drugmakers often extend that same price to commercial plans to simplify billing. That’s called "spillover pricing." Stanford Medicine estimates private insurers could save $200-250 billion over the next decade because of this ripple effect.

What about drug companies?
Pharmaceutical companies aren’t happy. They argue that lower prices hurt innovation. The industry group PhRMA claimed the program could cut $112 billion from R&D over 10 years. But the Office of Management and Budget called those numbers "significantly overstated."
Reality check: these companies still make money. Even with a 70% discount, Eliquis is still a $120-a-month drug. And with Medicare as a guaranteed buyer for 100 million people, volume offsets the lower price. Many manufacturers accepted the deals quietly. Only four filed lawsuits - and those were dismissed in August 2024. Appeals are coming, but the legal foundation is solid.
Drugmakers are also adjusting. Some are shifting focus to newer drugs that aren’t eligible yet. Others are bundling services - like patient support programs - to keep value high even as prices drop.
What’s next? The expansion plan
This isn’t a one-time event. The program is designed to grow.
- 2026: 10 drugs (already negotiated)
- 2027: 15 more drugs - including Farxiga and Stelara
- 2028: 15 more, plus the first Medicare Part B drugs (given in doctors’ offices, like cancer infusions)
- 2029 and beyond: 20 drugs per year
Part B is a bigger challenge. Right now, doctors get paid 6% above the drug’s average price. If that price drops, their income drops too. CMS is working on new payment models to make sure doctors don’t stop prescribing these drugs. By 2028, 45% of physician practices will need to change how they handle these medications, according to Medicare’s own advisory panel.
Why this matters for you, even if you’re not on Medicare
If you have private insurance, you’ll likely see lower prices too. Insurers often use Medicare’s negotiated prices as a benchmark. Pharmacy benefit managers are already updating their systems to reflect these new rates. You might not notice a change on your monthly bill right away, but over time, your premiums could stabilize - or even drop.
Even if you’re young and healthy, this program changes the whole system. It proves that the government can negotiate prices without collapsing the market. That sets a precedent. If future laws expand this to more drugs, or lower the eligibility age, you could be next.

Potential downsides and risks
Not everything is smooth sailing.
Some patient groups worry about therapeutic substitution - being forced to switch to a different drug just because it’s cheaper. If you’re stable on Xarelto, you don’t want to be pushed to a similar but less-tested drug. CMS says they consider clinical evidence before negotiating, but doctors and patients still need to be involved in treatment decisions.
Another risk: if drugmakers cut back on production or delay new versions to avoid eligibility, access could get tighter. The FTC has already started cracking down on "product hopping" - when companies make tiny changes to a drug just to extend exclusivity. That’s a good sign, but it’s still early.
And what about biosimilars? These are cheaper versions of biologic drugs. But uptake in the U.S. is still under 30%. Until that changes, many high-cost drugs will remain eligible for negotiation because they’re the only option. That’s a problem - not because of the negotiation, but because the market isn’t competitive enough.
What you should do now
If you’re on Medicare:
- Check your Part D plan’s formulary in late 2025. The new prices will be listed there.
- Ask your pharmacist if your drug is one of the 10 being negotiated.
- Don’t assume your copay stays the same - it will drop, but not always proportionally.
If you’re on private insurance:
- Keep an eye on your explanation of benefits. You might see lower prices appear in 2026.
- Ask your insurer if they’ve adopted Medicare’s negotiated rates.
- Use price comparison tools - many apps now show Medicare prices as a reference point.
If you’re a caregiver or advocate:
- Help seniors understand this isn’t a cut - it’s a correction.
- Push back if your provider tries to force a drug switch without medical justification.
- Track your out-of-pocket costs year over year. The savings will show up.
Final thoughts
This isn’t about punishing drug companies. It’s about fixing a broken system where one group - Medicare - was forced to pay inflated prices while everyone else negotiated. The Inflation Reduction Act didn’t invent price controls. It just gave Medicare the same power private insurers have had for years.
The results so far are clear: prices are falling. Savings are real. Patients are getting relief. And the system is adapting - slowly, but surely.
By 2028, when Part B drugs enter the picture, we’ll see if this model works for complex, clinic-based treatments. If it does, this could be the beginning of a new era - where drug prices finally reflect what’s fair, not just what’s profitable.
Which drugs are included in the first Medicare price negotiation round?
The first 10 drugs selected for negotiation in 2026 include Eliquis (apixaban), Jardiance (empagliflozin), Xarelto (rivaroxaban), Farxiga (dapagliflozin), Lyrica (pregabalin), Enbrel (etanercept), Humira (adalimumab), Stelara (ustekinumab), Repatha (evolocumab), and Leqvio (inclisiran). These are all high-cost, single-source medications with no generic alternatives and at least seven years on the market.
Will my Medicare Part D premiums go down because of this?
Yes, over time. The $98.5 billion in savings projected over 10 years will help reduce the overall cost of the Part D program. That can lead to lower premiums, especially as the program expands to more drugs. However, premiums are also affected by other factors like enrollment and administrative costs, so the drop won’t be immediate or dramatic in 2026.
Can drug companies refuse to negotiate?
No. Under the Inflation Reduction Act, manufacturers of selected drugs must participate. If they don’t respond or refuse to negotiate, they face a steep penalty - up to 95% of their sales in the U.S. being taxed. That’s a huge financial risk, so all 10 companies engaged in the process, even if they challenged it in court.
Why does this only apply to drugs that are 7+ years old?
The law was designed to avoid disrupting innovation. New drugs often have high R&D costs, and the 7-year (or 11-year for biologics) waiting period gives companies time to recoup investment before facing price negotiation. This balance aims to protect innovation while still tackling long-standing high prices.
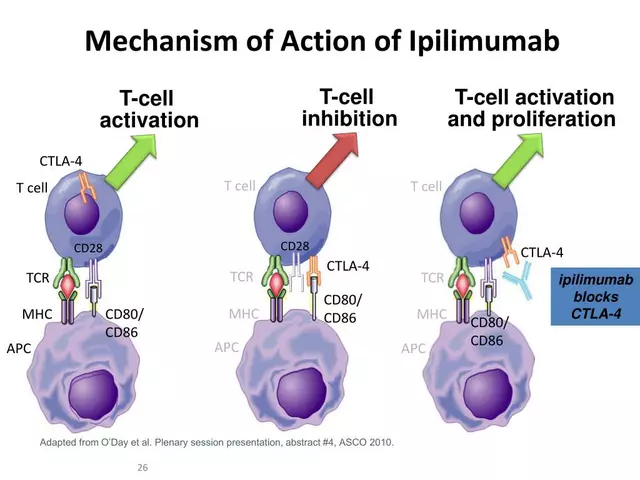
Does this affect drugs I get from my doctor’s office, like cancer treatments?
Not yet - but soon. The first 10 drugs are all taken orally (Part D). Starting in 2028, Medicare will begin negotiating prices for Part B drugs - those given in clinics, like infusions for cancer or autoimmune diseases. That’s a bigger challenge because it involves how doctors are paid, but the same negotiation principles will apply.
Will my private insurance plan match the new Medicare prices?
Many will. Private insurers often use Medicare’s negotiated prices as a benchmark because it’s a transparent, government-backed rate. This is called "spillover pricing." Some plans may adopt the lower price immediately; others may wait to see how it plays out. Either way, you’re likely to see lower costs over time.
Are there any drugs that won’t be eligible for negotiation?
Yes. Drugs with generic or biosimilar competitors are excluded. Also, new drugs under the 7-year (or 11-year) mark can’t be negotiated yet. Insulin and vaccines are also protected under separate rules. The program is designed to target only the most expensive, monopolized drugs - not all prescriptions.

Alicia Hasö
January 9, 2026 AT 10:36This is the kind of policy change that actually saves lives. I’ve seen seniors skip doses just to make their meds last - and now, for the first time, there’s real hope they won’t have to. A 70% drop on Eliquis? That’s not a discount, it’s justice.
My grandmother’s on Jardiance. She cried when I told her her monthly copay’s going from $180 to $45. She said, ‘I didn’t think I’d ever live to see this.’ We did. And we didn’t even have to riot.
Drug companies can cry all they want about innovation - but when your profit margin is built on people choosing between insulin and groceries, you’re not innovating. You’re exploiting.
This isn’t socialism. It’s basic fairness. Private insurers have been negotiating for decades. Medicare just got a seat at the table. That’s all.
I’m not saying it’s perfect. But it’s the first real step in decades. Let’s not ruin it by overcomplicating it.
Thank you to every lawmaker who stood up to the lobbyists. You changed lives today.
And to the folks saying ‘this will kill innovation’ - show me the last life-saving drug invented because of a $600 pill. I’ll wait.
Ashley Kronenwetter
January 10, 2026 AT 21:33The structural integrity of this negotiation framework is sound. The use of international price benchmarks and private insurer rebate data as anchors ensures that the Maximum Fair Price remains empirically grounded rather than politically arbitrary.
Furthermore, the exclusion of drugs with generic or biosimilar alternatives demonstrates a deliberate effort to avoid distorting market competition where it already exists.
The 7-year eligibility threshold is appropriately calibrated to balance innovation incentives with fiscal responsibility.
This model, if extended to Part B and scaled as planned, could serve as a template for other publicly funded health systems globally.
Aron Veldhuizen
January 11, 2026 AT 00:18Let’s be honest - this isn’t about fairness. It’s about power. The government just declared war on private enterprise under the guise of ‘saving money.’
What’s next? Will they start negotiating the price of your Tesla? Your Netflix subscription? Your therapist’s hourly rate?
These companies aren’t evil. They’re risk-takers. They invest billions, fail constantly, and occasionally create miracles like Eliquis - which, by the way, saved my dad’s life.
Now we punish success? We reward mediocrity? This is how empires collapse - not with a bang, but with a bureaucrat adjusting a spreadsheet and calling it ‘justice.’
And don’t give me that ‘private insurers negotiate’ line. They do it behind closed doors with kickbacks and secret rebates. At least this is transparent.
Wait - I just contradicted myself. Maybe I’m the problem.
Heather Wilson
January 12, 2026 AT 21:2179% discount? Let’s look at the math. If Eliquis costs $500 and now costs $120, that’s $380 saved per prescription. Multiply that by 1.2 million Medicare users. That’s $456 million in savings per month.
But here’s the catch - drugmakers will simply raise prices on non-negotiated drugs to compensate. They’ve done it before. Look at insulin in 2018. Then look at 2023. Prices went up. Same playbook.
Also, who’s paying for the administrative cost of negotiating 20 drugs a year? CMS staff? Lawyers? Consultants? That’s not free.
And what about the 45% of physician practices that have to restructure their billing? Are they being compensated? Or are we just shifting the pain from patients to providers?
This looks good on paper. But in practice? It’s a Rube Goldberg machine built on wishful thinking.
And don’t even get me started on ‘spillover pricing.’ That’s a fantasy. Private insurers will cherry-pick the lowest prices and ignore the rest. They always do.
Micheal Murdoch
January 13, 2026 AT 14:31Let’s remember why this matters: people are dying because they can’t afford their meds. Not because they’re lazy. Not because they’re irresponsible. Because the system is rigged.
For years, we’ve been told that drug prices are ‘market-driven.’ But when one company owns the only version of a drug for a decade, that’s not a market - that’s a monopoly.
This isn’t about hating pharmaceutical companies. It’s about hating a system that lets them charge what they want while families choose between medicine and rent.
And yes - the savings will ripple out. Private insurers will follow. Premiums will stabilize. Younger people will pay less. Even if you’re healthy now, this protects your future self.
Change feels scary when you’ve been told it’s impossible. But this? This is proof that we can fix broken things when we stop listening to the people who profit from the breakage.
Don’t let the noise drown out the quiet relief of a senior breathing easier because their pill doesn’t cost a week’s groceries.
Jeffrey Hu
January 14, 2026 AT 09:39Wait, so Medicare can negotiate now? But private insurers could always do it? So why didn’t they? Because they’re dumb? Or because they were getting kickbacks?
Also, did you know that the 10 drugs selected are ALL from big pharma - no startups? That’s because the law was written by lobbyists to target only the big fish. Small companies? Still screwed.
And the 7-year rule? That’s a loophole. Companies just tweak the formula and relaunch as ‘new’ - called product hopping. FTC is on it, but barely.
Also, why no insulin? Oh right - because they’re scared of backlash. But they’re negotiating Jardiance? That’s a diabetes drug. So why not insulin? Hypocrisy.
And don’t tell me about ‘spillover pricing.’ My insurance didn’t drop a cent last year when Medicare cut prices on 5 drugs. Still paying full price. So yeah, good luck with that.
Meghan Hammack
January 16, 2026 AT 05:18I just talked to my mom. She’s on Humira. Used to be $700 a month. Now? $180. She said she’s going to start saving again - for the first time in 10 years.
She cried. I cried. We didn’t even say anything. Just held each other.
This isn’t policy. This is love in action.
RAJAT KD
January 16, 2026 AT 23:39Finally. The U.S. caught up with the rest of the world. Canada, Germany, Australia - they’ve had this for decades. Why did it take so long? Because the lobby was too strong. Now it’s broken. Good.
Stop pretending this is radical. It’s basic. Every civilized country does this. We’re late. But we’re here.
Matthew Maxwell
January 18, 2026 AT 19:46This is the slippery slope. Next, they’ll come for your car insurance. Your rent. Your coffee.
They call it ‘fair pricing.’ I call it theft. The government is now a price setter - not a regulator. That’s not democracy. That’s authoritarianism with a smile.
And don’t tell me about ‘private insurers negotiate.’ They do it with contracts. This is coercion. Under threat of 95% tax. That’s not negotiation. That’s extortion.
And you call this ‘justice’? What about the shareholders? The employees? The scientists who spent 15 years developing these drugs? Their dreams are now a spreadsheet line item.
This is how socialism begins. With a ‘good cause.’ Then it never stops.
Lindsey Wellmann
January 20, 2026 AT 04:46OMG I’m literally crying 😭
My aunt took Eliquis. She had to sell her jewelry to afford it. Now? She’s going to Hawaii next year. I’m so proud of this country 🇺🇸💖
Drug companies can cry all they want - they made billions anyway. This is just them paying their fair share. 💅✨
Also, can we make this law apply to pet meds next? My dog’s on the same stuff as my uncle. He’s a good boy. He deserves cheaper meds too 🐶💕
tali murah
January 21, 2026 AT 17:38Oh wow, another feel-good policy that ignores economic reality. Let’s celebrate the government ‘saving’ $98 billion - while ignoring that drugmakers will just cut R&D in areas that don’t have guaranteed buyers.
And let’s pretend that ‘spillover pricing’ is real. It’s not. Private insurers will use Medicare’s price as a floor, not a ceiling - meaning they’ll pay less, but not as much as you think.
Also, 79% discount? That’s only possible because these drugs were grossly overpriced to begin with. So what? That’s capitalism. You don’t get to punish success because you’re mad you couldn’t afford it.
And don’t even get me started on the lawsuits being dismissed. Of course they were. The courts are packed with appointees who hate corporate power.
This isn’t reform. It’s revenge dressed as policy.
Jenci Spradlin
January 22, 2026 AT 08:33so like… eliquis went from 500 to 120? that’s wild. my cousin just got on it and was freakin’ out about the cost. now she’s chillin’. also, my mom’s on jardiance and she’s gonna start eating out again. no joke.
also, why is everyone so mad? these companies made billions. they’re not gonna go broke. they’ll just make more new drugs. duh.
also, if my private insurance doesn’t drop prices, i’m switching plans. easy.
Elisha Muwanga
January 23, 2026 AT 06:05Let’s not pretend this is about healthcare. This is about control. The federal government just asserted its right to dictate pricing on private enterprise. That’s not ‘fairness.’ That’s tyranny wrapped in a ribbon.
And don’t tell me about ‘other countries do it.’ We’re not Canada. We’re not Germany. We’re the United States - where innovation thrives because you’re allowed to profit from it.
Now we’re punishing success. Next, they’ll regulate your Netflix subscription. Your Amazon Prime. Your Spotify.
And don’t give me that ‘but people are suffering’ line. That’s not a justification for socialism. That’s an emotional manipulation tactic.
This is the beginning of the end for American capitalism. And I’m not okay with it.
Alicia Hasö
January 25, 2026 AT 05:41And yet - the lawsuits failed. The data shows savings. The patients are breathing easier. And the drugmakers? They’re still making billions.
So maybe ‘tyranny’ is just what it sounds like when the powerful lose their grip.
And yes - if this works for Part B in 2028, we’ll be talking about cancer drugs dropping 70%. That’s not the end of capitalism. That’s the beginning of sanity.