When you pick up a new prescription, the small paper insert that comes with it isn’t just paperwork-it could save your life. These are called Medication Guides, and they’re not optional. The FDA requires them for drugs with serious, preventable risks. But most people glance at them and put them away. That’s a mistake. These guides aren’t written for lawyers or doctors. They’re written for you. And if you learn how to read them right, you’ll know exactly what to watch for, when to call your doctor, and what tests you need.
What Makes a Medication Guide Different?
Not all drug information is the same. There’s the full prescribing info for doctors, the little leaflet inside the bottle, and then there’s the Medication Guide. This one is special. It’s only given out for medications that can cause serious harm-like liver damage, dangerous drops in blood cells, or life-threatening allergic reactions. Right now, about 150 different guides exist for drugs across 30 categories, from antidepressants to blood thinners to cancer treatments. The FDA made these mandatory in 1997 because they found that when patients understand the risks, fewer bad things happen.These guides aren’t written in medical jargon. The law says they must be at a 6th to 8th grade reading level. That means short sentences, clear headings, and no confusing terms. And they’re formatted consistently. Every guide has the same seven sections. That’s intentional. The FDA wants you to find the critical info fast-no matter which drug you’re taking.
The Three Sections That Matter Most
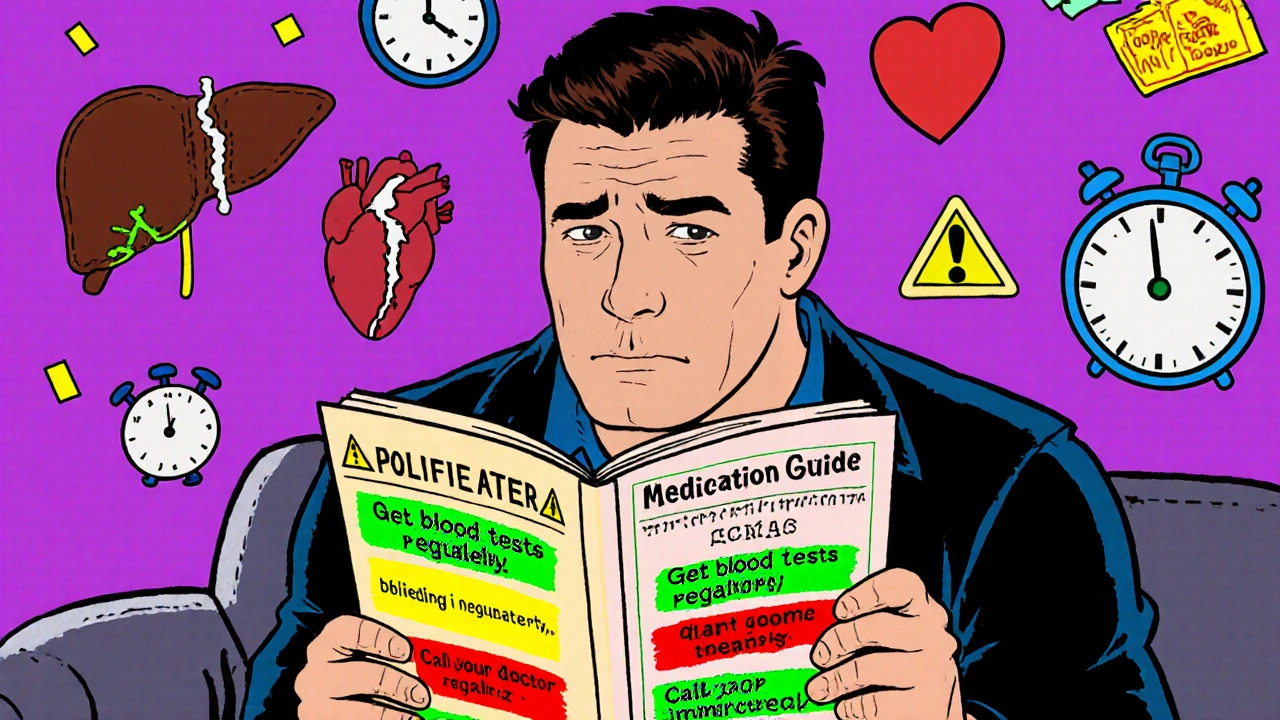
You don’t need to read every word. Focus on these three parts:- What is the most important information I should know about [drug name]? This is where the FDA puts its strongest warnings. Look for phrases like “can cause serious liver damage” or “may lead to life-threatening infections.” This section often includes black box warnings-the highest level of risk alert. If your drug has one, this is where it’s explained in plain language.
- What are the possible or reasonably likely serious side effects of [drug name]? This is the monitoring section. Here, they tell you exactly what to check for and how often. For example, the guide for the arthritis drug tofacitinib says: “Get your blood tested regularly to check for changes in blood cell counts.” It doesn’t say “maybe check your blood.” It says “get tested.” That’s a command, not a suggestion.
- What should I tell my healthcare provider before taking [drug name]? This tells you what conditions or medications could make your drug dangerous. If you have liver disease, kidney problems, or are taking another drug that interacts with it, this section will tell you. If you have any of these, you need to talk to your doctor before you start.
Don’t skip the “How should I take [drug name]?” section either. It often includes monitoring schedules. For example, the blood thinner warfarin (Coumadin) guide says: “Your INR should be checked at least once a month. If your dose changes, check it more often.” It even lists symptoms that mean you need to go to the ER: “unusual bruising or bleeding that lasts a long time.”
Numbers Tell the Real Story
Vague language like “may cause dizziness” is useless. The best guides use real numbers. The clozapine (Clozaril) guide says: “About 1 in 200 people taking clozapine may develop a condition called agranulocytosis.” That’s concrete. You can understand that. And it comes with a clear action: “You’ll need weekly blood tests for the first 6 months.”Research from Harvard Medical School shows that when guides use numbers instead of vague terms, patient understanding improves by 47%. That’s huge. If your guide says “some people get headaches,” ask your pharmacist: “How many?” If they don’t know, the guide might not be helping you.
Red Flags: Words That Mean Stop and Call
The Agency for Healthcare Research and Quality (AHRQ) identified seven phrases that should make you pause. If you see any of these in your guide, highlight them:- “Get blood tests regularly”
- “Call your doctor immediately if”
- “Do not stop taking without talking to your doctor”
- “Avoid sunlight exposure”
- “Do not drink alcohol”
- “May impair driving ability”
- “Keep all scheduled appointments”
These aren’t suggestions. They’re safety rules. For example, if your antidepressant guide says “Pay close attention to any sudden changes in mood, behavior, or thoughts,” that’s not about feeling a little sad. It’s about suicidal thoughts or extreme agitation-especially in the first 4 to 6 weeks. That’s when the risk is highest.
How to Actually Use This Info
Reading the guide once isn’t enough. Here’s how to make it work:- Use the 3-2-1 Method: Spend 3 minutes reading it before you take your first dose. Review it for 2 minutes every time you refill. And spend 1 minute checking for updates during treatment. The FDA requires manufacturers to update guides within 30 days of new safety info-and 92% did so in 2022.
- Highlight and circle: Grab a yellow highlighter and mark every word like “test,” “monitor,” “check,” or “measure.” Circle any time frame: weekly, monthly, immediately. Underline emergency symptoms in red. This turns a wall of text into a visual checklist.
- Build a monitoring calendar: If your guide says “blood tests every 3 months,” write those dates on your phone calendar. Set reminders. The University of Michigan found that patients who did this had 68% fewer adverse events.
- Use the traffic light system: Green = normal, yellow = call your doctor, red = go to the ER. Write down your guide’s symptoms under each color. For warfarin: green = no bruising, yellow = small bruise, red = bleeding that won’t stop.
Pharmacists report that when they physically point out the monitoring section and explain it in under 90 seconds, patients are 82% more likely to follow the testing schedule. You don’t need to be a doctor to understand this. You just need to know where to look.
What If You Don’t Get the Guide?
The law says you must get a Medication Guide every time you fill your prescription. But a 2022 audit found that 41% of independent pharmacies didn’t always give them out. If you don’t get one, ask for it. Say: “I need the FDA Medication Guide for this drug.” If they say they don’t have it, call the pharmacy’s corporate office or check DailyMed (the NIH’s official database). You can download and print the current guide for free.More than 12 million guides were downloaded from DailyMed in 2022. The most popular? Diabetes and heart medications. If your drug isn’t on the list, it might not need one. But if it’s a high-risk drug-like an immunosuppressant, anticoagulant, or psychiatric medication-it should have one.
What’s Changing in 2025?
The system is getting better. By 2025, all drugs with Risk Evaluation and Mitigation Strategies (REMS) will need a Medication Guide. That’s expanding coverage from 42 to 127 drugs. The FDA is testing QR codes on packaging that link directly to the guide. Some companies are using AI to personalize guides based on your age, other meds, and health history. Early results show patients understand their risks 63% better.But there’s still a big problem: 40% of U.S. adults struggle with health literacy. Even the clearest guide won’t help if you can’t understand it. That’s why future guides will include pictograms-simple icons showing when to test, what symptoms to watch for, and when to call for help. By 2026, these will be required.
Why This Matters More Than You Think
The FDA studied 500 patients and found that those who followed their guide’s monitoring advice had 32% fewer bad reactions. That’s not small. It means fewer hospital visits, fewer emergency trips, and fewer missed days of work. It also means your doctor can adjust your treatment safely because they know you’re tracking the right things.Medication Guides are your personal safety net. They’re not meant to scare you. They’re meant to give you control. You don’t have to trust your doctor blindly. You don’t have to guess what’s normal. The guide tells you exactly what to watch for-and when to act.
Do I need to read the Medication Guide every time I refill my prescription?
Yes. Manufacturers are required to update guides within 30 days if new safety info comes out. Even if your prescription hasn’t changed, the risks might have. Reviewing it every refill takes just 2 minutes and could catch an important update-like a new warning about alcohol use or a change in blood test frequency.
What if I don’t understand a word in the guide?
Don’t guess. Ask your pharmacist or doctor. They’re required to explain it. If you’re not comfortable asking in person, call the drug manufacturer’s patient help line-every guide lists one. For example, the guide for Humira includes a toll-free number for questions about TB testing. You’re not expected to know medical terms. You’re expected to ask.
Are Medication Guides the same as the instructions on the pill bottle?
No. The bottle label tells you how much to take and how often. The Medication Guide tells you what could go wrong and what you need to do to prevent it. One is about dosing. The other is about safety. You need both.
Can I rely on online reviews or forums instead of the guide?
No. Online reviews talk about side effects, but they don’t tell you what’s serious, how often it happens, or what monitoring you need. The Medication Guide is the only source that’s reviewed and approved by the FDA. It’s the only one that gives you official, evidence-based monitoring instructions.
What if I miss a blood test or monitoring appointment?
Call your doctor right away. Don’t wait. For some drugs, like clozapine or warfarin, missing a test can be dangerous. Your doctor may need to pause your medication until the test is done. The guide says “get tested regularly” for a reason-it’s not optional. Missing one test increases your risk of a serious reaction.
Do all prescription drugs have Medication Guides?
No. Only drugs with serious, preventable risks have them. Common meds like antibiotics, blood pressure pills, or birth control usually don’t. But if you’re taking a drug for depression, autoimmune disease, cancer, or blood clotting, you almost certainly will. If you’re unsure, ask your pharmacist: “Does this drug have an FDA Medication Guide?”
Can I get a digital copy of my Medication Guide?
Yes. Go to DailyMed.nlm.nih.gov and search by drug name. You can download, print, or save it to your phone. Many pharmacies also email guides when you order online. Keep a digital copy in your health app or notes. It’s easier to check than a paper one that gets lost in a drawer.

DENIS GOLD
November 29, 2025 AT 00:06Oh wow, another government pamphlet telling me how to live my life. Next they'll make me read the instructions on my toothpaste. 'Warning: May cause enamel removal if used with excessive enthusiasm.' 🤡
Ifeoma Ezeokoli
November 29, 2025 AT 16:50Y’all, this is actually beautiful. 🌍✨ I come from a place where most folks don’t even get pamphlets, let alone ones written in plain English. This feels like someone finally said, 'Hey, you matter.' Let’s make sure every pharmacy in every town-especially the rural ones-gives this out without asking twice. ❤️
Daniel Rod
November 30, 2025 AT 01:03It’s wild how we treat medicine like a magic spell instead of a tool. 🤔 We swallow pills like they’re wishes and then act shocked when things go wrong. This guide isn’t about fear-it’s about agency. You’re not a patient. You’re a partner in your own survival. And if you’re not reading this? You’re letting someone else hold the reins. 🫶
gina rodriguez
December 1, 2025 AT 06:51I always keep my guides in my phone notes. I highlight the red flags and set reminders for blood tests. It’s just 2 minutes a refill-but it’s the difference between ‘I’m fine’ and ‘I almost ended up in the ER.’ You got this. 💪
Sue Barnes
December 3, 2025 AT 03:07If you’re not reading these, you’re an idiot. Plain and simple. People die because they think ‘maybe it’s just a headache’ instead of ‘this is a black box warning.’ Stop being lazy. Your life isn’t a suggestion box.
jobin joshua
December 5, 2025 AT 00:52Bro, I read this and then went to my mom’s pharmacy-she’s on warfarin-and they didn’t give her the guide! I called the corporate office and they sent it the next day. Also, I sent her a screenshot with emojis: 🚨🔴❗️
Sachin Agnihotri
December 6, 2025 AT 05:01Wait, so you’re telling me… the FDA actually made something that’s easy to read? And it’s not just a legal loophole? I’m… honestly touched. Like, I didn’t think they could do this. And now I’m gonna print mine out and stick it on my fridge. With a magnet. Because why not?
Diana Askew
December 7, 2025 AT 13:18They’re lying. This is all a ploy to get you to trust Big Pharma. The real danger is the QR codes-they’re tracking you. And the ‘AI personalized guides’? That’s just the government prepping for mandatory health surveillance. Next thing you know, your insulin pump will send your location to the FDA. 🕵️♀️
King Property
December 8, 2025 AT 04:12You people are missing the point. This isn’t about reading guides-it’s about systemic failure. The FDA doesn’t care about you. They care about liability. The fact that 41% of pharmacies don’t hand these out? That’s not negligence-that’s policy. And the ‘6th grade reading level’? That’s condescending. You think the average person can’t handle ‘hepatotoxicity’? They can. But they’re being treated like children so the drug companies don’t get sued. This isn’t empowerment. It’s damage control dressed up like a self-help book. And you’re all drinking the Kool-Aid.