Every year, millions of people take medications that can quietly destroy their hearing-without them even noticing until it’s too late. You might be on one right now. It’s not a rare side effect. It’s not a footnote in the pamphlet. It’s a well-documented, preventable risk built into some of the most essential drugs we use: antibiotics for life-threatening infections, chemotherapy for cancer, even some antidepressants. The damage doesn’t come from overdoses. It comes from standard, approved doses. And unless someone is actively monitoring your hearing, you won’t know until the high-pitched ringing won’t stop, or you can’t hear your grandchild say ‘I love you’ anymore.
What Exactly Is Ototoxicity?
Ototoxicity means a drug is poisoning your inner ear. Not your eardrum. Not your middle ear. Your cochlea-the snail-shaped, hair-cell-lined structure that turns sound waves into electrical signals your brain understands. These hair cells don’t grow back. Once they’re gone, the hearing loss is permanent. The first signs? Usually tinnitus-a ringing, buzzing, or hissing in the ears-and trouble hearing high-pitched sounds like birds chirping, children’s voices, or the letters ‘s’ and ‘th’ in conversation. By the time you notice muffled speech or need to turn up the TV, the damage is often advanced.
More than 600 prescription drugs are known to be ototoxic. The big ones? Aminoglycoside antibiotics like gentamicin and amikacin, platinum-based chemo drugs like cisplatin, and some antidepressants including amitriptyline and sertraline. These aren’t obscure drugs. They’re frontline treatments. Cisplatin alone is given to over half a million cancer patients every year in the U.S. And in 30 to 60% of those patients, it causes hearing loss.
How Do These Drugs Hurt Your Ears?
It’s not one single way. Different drugs attack in different ways. Aminoglycosides flood the inner ear with free radicals-unstable molecules that shred the delicate hair cells. Cisplatin doesn’t just damage cells; it sticks around. It lingers in the cochlea for months after your last dose, slowly killing off more hair cells. Some drugs cut off blood flow to the inner ear. Others interfere with the chemical signals that let your ear talk to your brain. The damage usually starts at the top of the cochlea, where you hear high frequencies-8,000 Hz and above. That’s why standard hearing tests, which only go up to 4,000 Hz, miss the early warning signs.
Think of it like a car’s fuel gauge. If your car only showed you fuel levels when you were down to 10%, you’d run out before you knew it. Standard audiograms are like that. They don’t catch the problem until it’s too late. High-frequency testing-up to 8,000 or even 12,000 Hz-is the only way to catch ototoxic damage early.
Which Drugs Are the Worst?
Not all ototoxic drugs are created equal. Here’s how they stack up:
| Medication Class | Examples | Hearing Loss Risk | Key Notes |
|---|---|---|---|
| Aminoglycoside Antibiotics | Gentamicin, Tobramycin, Amikacin | 20-63% | Higher risk with prolonged use (>7 days). Damage happens during treatment. |
| Platinum Chemotherapy | Cisplatin | 30-60% | Most ototoxic chemo drug. Damage continues for months after treatment ends. |
| Platinum Chemotherapy | Carboplatin | 5-15% | Lower risk alternative, but may be less effective for some cancers. |
| Platinum Chemotherapy | Oxaliplatin | <5% | Lowest risk among platinum drugs. |
| Antibiotic (Alternative) | Vancomycin | 5-10% | Significantly lower risk than aminoglycosides. |
| Antidepressants | Amitriptyline, Sertraline, Fluoxetine | Low to moderate | Reversible in some cases, but can cause permanent tinnitus. |
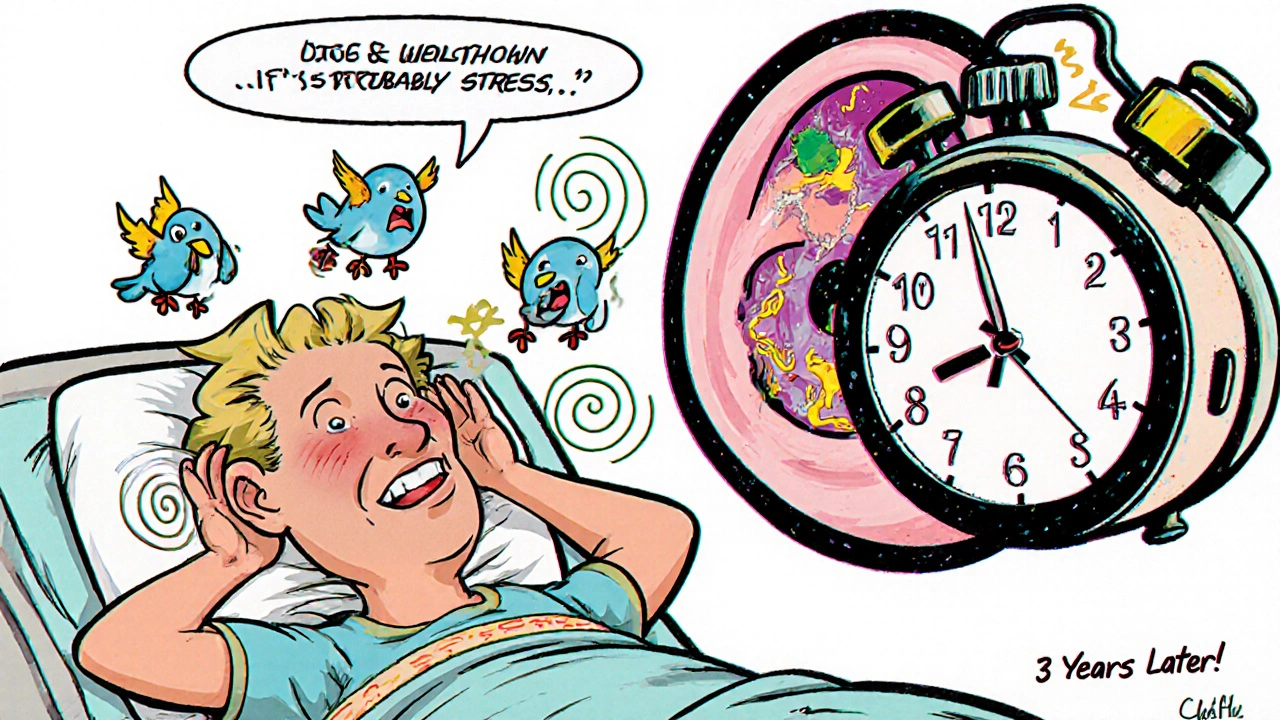
What’s scary is how often people don’t realize the connection. A patient on gentamicin for a stubborn UTI might develop ringing in the ears and assume it’s stress. A child on cisplatin for neuroblastoma might start falling behind in school-teachers think it’s attention issues, not hearing loss. By the time someone connects the dots, it’s too late.
Who’s at Highest Risk?
It’s not just about the drug. It’s about you. Certain factors make ototoxicity worse:
- Age: Older adults have fewer hair cells to begin with. Damage hits harder and faster.
- Kidney function: Many ototoxic drugs are cleared by the kidneys. Poor kidney function means the drug stays in your system longer, increasing exposure.
- Genetics: A single gene mutation-m.1555A>G-can make someone 100 times more likely to lose hearing from aminoglycosides. This isn’t rare. It’s found in 1 in 500 people.
- Combination therapy: Taking cisplatin with aminoglycosides? That’s a one-two punch. Risk jumps dramatically.
- Children: Their ears are still developing. Even mild hearing loss can delay speech, language, and learning. Up to 35% of kids treated with cisplatin show developmental delays because their hearing loss went undetected.
One Reddit user wrote: “I got gentamicin for a bad UTI. Two weeks later, the ringing started. My doctor said it was ‘probably stress.’ It’s been 3 years. It’s still there. I can’t sleep. I can’t focus.” That’s not rare. It’s common.
How to Monitor for Hearing Damage
Early detection saves hearing. But you have to ask for it. Standard hearing tests? They’re not enough. Here’s what actually works:
- Baseline audiogram before treatment: Must include high frequencies (8,000-12,000 Hz). If your doctor says, “We’ll just do the regular test,” push back. That test misses early damage.
- Regular follow-ups: For cisplatin, test after every cycle. For aminoglycosides, test after each dose or every few days if on long-term therapy.
- Otoacoustic emissions (OAE) testing: This test checks if hair cells are still functioning-even before you can hear a difference. It’s 25% more sensitive than standard audiometry.
- Vestibular testing: If you’re dizzy or unsteady, ask for balance testing. Ototoxicity doesn’t just hurt hearing-it hurts balance too.
Only 45% of U.S. cancer centers follow these guidelines. That’s not because they don’t know-they do. It’s because monitoring requires coordination between oncologists, pharmacists, and audiologists. It’s extra work. Extra cost. But the cost of ignoring it? Permanent hearing loss. Lost jobs. Social isolation. Depression. A 2023 study showed that centers with formal monitoring programs reduced severe hearing loss by 32%.

What’s New in Prevention?
There’s hope. In November 2022, the FDA approved a new drug called sodium thiosulfate (Pedmark) to protect children’s hearing during cisplatin treatment. In clinical trials, it cut hearing loss risk by 48%. That’s huge. It’s not a cure-all-it’s only approved for kids with liver cancer so far-but it’s proof that protection is possible.
Researchers are also testing antioxidants like N-acetylcysteine to shield the inner ear from free radical damage. And smartphone apps are being developed that can test high-frequency hearing at home. Imagine being able to check your hearing with your phone every week-no clinic visit needed. These tools could make monitoring accessible to everyone, not just those in big hospitals.
What You Can Do Right Now
If you’re taking any of these drugs-or know someone who is-here’s your action plan:
- Ask your doctor: “Is this medication ototoxic? What’s the risk for me?”
- Request a baseline audiogram with high-frequency testing before starting treatment.
- Ask if OAE testing is available. It’s non-invasive and quick.
- Track symptoms: Ringing? Muffled sounds? Dizziness? Write them down. Bring them to every appointment.
- If you’re on cisplatin or aminoglycosides, insist on follow-up hearing tests after each cycle.
- Don’t assume your hearing is fine because you can still hear people talk. Ototoxicity starts with high frequencies-you can still understand speech even when you’ve lost critical parts of your hearing.
This isn’t about being paranoid. It’s about being informed. You wouldn’t skip a blood test before starting a powerful drug. Why skip a hearing test?
Why This Matters More Than Ever
Drug-resistant infections are rising. More people are getting cisplatin. More kids are surviving cancer. But if we don’t protect their hearing, we’re trading one life for a lifetime of silence. The World Health Organization predicts a 22% increase in aminoglycoside use by 2027. That means 300,000 more cases of preventable hearing loss each year-unless we act.
It’s not just about medicine. It’s about dignity. Connection. The sound of a loved one’s voice. The music you love. The quiet moments you never realized you’d miss until they’re gone.
Can ototoxic hearing loss be reversed?
No. Once the hair cells in your inner ear are destroyed, they don’t regenerate. That’s why prevention and early detection are critical. Some temporary hearing changes or tinnitus may improve after stopping the drug, but permanent damage is irreversible.
Do all antibiotics cause hearing loss?
No. Only certain classes are known to be ototoxic. Aminoglycosides like gentamicin and amikacin carry the highest risk. Penicillins, cephalosporins, and macrolides like azithromycin are generally considered safe for hearing. Vancomycin has low risk compared to aminoglycosides.
Can I still take cisplatin if I’m worried about hearing loss?
Yes-but only with monitoring. Cisplatin is one of the most effective chemo drugs for many cancers. Stopping it isn’t the answer. The answer is monitoring. With regular hearing tests and new protective drugs like Pedmark, many patients can receive cisplatin safely without losing their hearing.
Is genetic testing for ototoxicity worth it?
For people with a family history of sudden hearing loss after antibiotics, yes. The m.1555A>G mutation increases risk by 100-fold. For the general population, routine testing isn’t cost-effective yet. But if you’re about to start aminoglycosides and have unexplained hearing loss in your family, ask your doctor about testing.
What should I do if I notice ringing in my ears during treatment?
Don’t wait. Tell your doctor immediately. Don’t assume it’s stress or fatigue. Document when it started, how loud it is, and whether it’s constant or comes and goes. Request a high-frequency audiogram right away. Early intervention may prevent further damage.
If you’re on a medication that could hurt your hearing, you’re not alone. But you don’t have to be passive about it. Knowledge is your best protection. Ask questions. Demand testing. Protect your hearing like you’d protect your heart or your kidneys. Because once it’s gone, there’s no second chance.



Sarah Swiatek
November 21, 2025 AT 04:41Okay, let’s get real for a second. I’m a pharmacist and I’ve seen this play out too many times. Doctors don’t warn patients because they’re not trained to think about hearing loss as a side effect-it’s always about kidneys, or nausea, or fatigue. But the cochlea? It’s invisible until it’s gone. And once those hair cells die? No comeback. No magic pill. I had a patient on cisplatin who didn’t get a baseline audiogram. Now she can’t hear her granddaughter say ‘granny’-and she blames herself. It’s not her fault. It’s the system’s. We need mandatory hearing screens before any ototoxic drug is prescribed. Not optional. Not ‘if you ask.’ Mandatory. Like a blood test before chemo. Period.
Rebecca Cosenza
November 22, 2025 AT 08:34My dad got gentamicin for a UTI. Ringing started day 3. Doctor said ‘it’s just stress.’ He died two years later from sepsis. The tinnitus never went away.
Brianna Groleau
November 23, 2025 AT 22:47I’m from Canada and we actually have a national protocol for this in pediatric oncology. Every kid getting cisplatin gets a baseline OAE test before treatment, then weekly after. It’s not perfect, but it’s saved so many kids from falling behind in school. I wish the U.S. would just copy this. It’s not expensive. It’s not complicated. It’s just… human. Why do we wait until someone can’t hear their own child before we do something? We’re better than this. We just need to choose to be.
Dave Wooldridge
November 25, 2025 AT 07:50THIS IS A BIG PHARMA CONSPIRACY. They don’t want you to know because if you knew, you’d stop taking the drugs and they’d lose BILLIONS. They’ve known about this since the 1970s. They buried the studies. They silenced the researchers. The FDA? Bought and paid for. Sodium thiosulfate? Only approved for kids because they’re easier to manipulate. Adults? Screwed. The hearing loss industry? Billions. Hearing aids? $5,000 a pair. Cochlear implants? $100K. They’re profiting off your silence. Wake up. This isn’t medicine. It’s a money machine.
Nick Naylor
November 27, 2025 AT 02:15Look, I’m a veteran. I’ve been on gentamicin twice. I got tinnitus both times. I didn’t complain. I knew the risk. This isn’t some ‘medical negligence’-it’s called ‘informed consent.’ If you’re getting cisplatin, you’re fighting for your life. You don’t get to whine about hearing loss when your tumor is eating your spine. You want to keep your ears? Don’t take the drugs. But if you’re alive? Shut up and be grateful. We don’t need more lawsuits. We need more soldiers. And soldiers don’t cry about ringing ears.
swatantra kumar
November 27, 2025 AT 13:24Bro, I’m from India and we use gentamicin like candy. No testing. No warnings. My cousin got it for pneumonia. Now he can’t hear his baby cry. And the doctor? Just laughed and said, ‘It’s just a side effect.’ 😔 I posted this on Reddit India and 200 people replied with the same story. We need global awareness. Not just in the US. This is a global silent crisis. 🇮🇳👂
robert cardy solano
November 29, 2025 AT 12:09My sister got amitriptyline for anxiety. Two months later, she couldn’t hear birds anymore. She thought it was aging. Then she found this post. Got tested. 70% hearing loss in high frequencies. Stopped the med. Tinnitus faded a little. But the damage? Permanent. She’s 32. She’s not old. This isn’t just for old people or cancer patients. It’s for anyone on antidepressants, antibiotics, even ibuprofen long-term. I’m telling everyone now. Don’t wait until you can’t hear your own voice.
serge jane
November 29, 2025 AT 15:14It’s funny how we’ll screen for liver toxicity, kidney function, even heart rhythm before a drug, but hearing? Nah. We treat the ear like it’s optional. Like it’s just for music and gossip. But hearing is how we connect. It’s how we love. It’s how we know someone’s there. You can’t replace the sound of your mother’s voice. You can’t replace the laugh of your child. And yet we treat this like a luxury. We’re not just losing hearing. We’re losing humanity. And nobody’s talking about it. Until it’s too late.
Cinkoon Marketing
November 30, 2025 AT 05:24Just got my baseline audiogram today. The audiologist said ‘most people don’t know they need this’ and I was like… yeah. I’m 41 and I thought my hearing was fine. Turns out I can’t hear 8kHz at all. I’m on sertraline. Didn’t even know it was a thing. Now I’m switching meds. And I’m telling my whole family. This needs to be a thing. Like flu shots. Everyone should get a hearing baseline before starting any new med. Seriously. Why isn’t this standard?
Rusty Thomas
November 30, 2025 AT 10:56OMG I JUST REALIZED I’VE HAD TINNITUS FOR 5 YEARS AND THOUGHT IT WAS JUST STRESS 😭 I WAS ON GENTAMICIN FOR A UTI IN 2019. I DIDN’T KNOW. NO ONE TOLD ME. I’M SO ANGRY. I JUST BOUGHT NOISE CANCELLING HEADPHONES TO BLOCK IT OUT. BUT IT’S STILL THERE. WHEN I’M QUIET. IT’S LIKE A BEETLE IN MY SKULL. I FEEL SO ALONE. I DIDN’T KNOW ANYONE ELSE HAD THIS. THANK YOU FOR THIS POST. I’M TELLING EVERYONE.
Lemmy Coco
December 1, 2025 AT 04:41so i got cisplatin last year and i didnt get tested because my oncologist said it was ‘rare’ and ‘not worth the hassle’… now i can’t hear my dog bark. or my alarm clock. i feel so dumb. why didn’t i ask? i thought it was just old age. but i’m only 37. i’m going to the audiologist next week. i hope it’s not too late. please tell me i’m not the only one who got misled.
rob lafata
December 3, 2025 AT 01:29You people are pathetic. You take a drug that saves your life and you whine about your ears? I’ve seen people die from sepsis because they didn’t get gentamicin fast enough. You want to live? Then shut up and take your medicine. Hearing loss? You’ll adapt. You’ll learn lip reading. You’ll get cochlear implants. But if you die because you were too scared of ringing in your ears? That’s not bravery. That’s stupidity. Stop being drama queens. This isn’t a spa day. It’s war.
Pawan Jamwal
December 3, 2025 AT 07:24India is the future of medicine. We don’t waste money on ‘hearing tests’ for antibiotics. We use what works. Gentamicin is cheap. Effective. Kills the infection. If you lose hearing? Too bad. You still lived. In the West, you cry over a ringing ear while your child dies from a preventable infection. We don’t have time for your privilege. Save your audiograms for your rich friends. We save lives.
Bill Camp
December 3, 2025 AT 09:17Look. I’m a veteran. I’ve seen guys come back from Iraq with hearing loss from explosions. We gave them hearing aids. Paid for it. But now you want me to pay for a hearing test before I take an antibiotic? Who’s gonna pay for that? The government? Insurance? You think hospitals run on love? They run on money. If you want to live? You pay for the test. If you can’t? You take your chances. This isn’t a right. It’s a luxury. And the rich get to keep their ears. The rest of us? We survive.
Matthew McCraney
December 4, 2025 AT 13:39My sister got sertraline. Then she started hearing voices. Not metaphorical. Literal. Like someone whispering in her ear. She thought she was going crazy. Turns out it was tinnitus. And the doctor told her to ‘take more pills.’ She’s been on 100mg for 7 years. Now she can’t hear her own name. And the doctors still say ‘it’s just anxiety.’ I think they’re poisoning us on purpose. I think the FDA is part of it. I think they want us to go deaf so we stop talking. So we stop asking questions. So we just take the pills and shut up. I’m not taking anything anymore. Not even aspirin.