Vitamin A Intake Calculator for Pregnancy
This tool helps you calculate your daily vitamin A intake from food and supplements to ensure you're staying safely under the recommended 10,000 IU limit during pregnancy. Remember: only preformed vitamin A (retinol) is dangerous during pregnancy.
Daily Vitamin A Sources
What Makes Vitamin A Dangerous During Pregnancy?
Most people think of vitamin A as a harmless nutrient-good for vision, skin, and immunity. But when it comes to pregnancy, vitamin A isn’t just a supplement. It’s a powerful drug that can cause irreversible birth defects. The difference isn’t about quantity alone-it’s about form. Preformed vitamin A (retinol, retinyl palmitate, retinaldehyde) is stored in the liver and can build up to toxic levels. Even a daily dose over 10,000 IU during early pregnancy can trigger major fetal malformations. That’s less than two servings of beef liver.
It’s not just supplements. Many prenatal vitamins contain retinyl palmitate, and fortified foods like cereals and dairy products add up. One 2022 Consumer Reports analysis found that 78% of prenatal vitamins include preformed vitamin A, averaging 2,565 IU per serving. That’s not dangerous on its own-but when you add in liver, fish oil, and fortified foods, it’s easy to cross the line without realizing it.
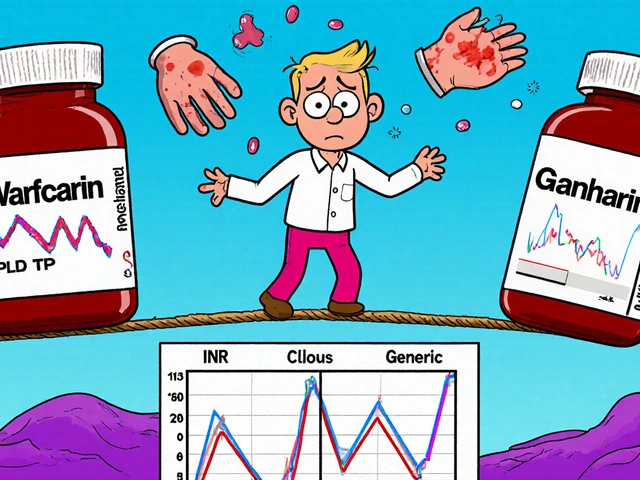
The Real Culprits: Prescription Retinoids
If you’re taking isotretinoin (Accutane®), you’re already aware of the risks. But the numbers are still shocking: 20-35% of pregnancies exposed to isotretinoin in the first trimester result in major birth defects. These aren’t rare anomalies. They’re systemic-heart defects, brain malformations, cleft palates, ear and eye abnormalities. The FDA’s iPLEDGE program was created to stop this. It requires two negative pregnancy tests, monthly counseling, and two forms of contraception. And yet, in 2021, 68% of isotretinoin-exposed pregnancies happened because patients didn’t follow the rules.
It’s not just isotretinoin. Etretinate (Tigason®) sticks around in the body for months-up to 120 days. That means even if you stop taking it, you’re still at risk. Acitretin, used for psoriasis, requires a two-year waiting period after stopping before you can safely try to conceive. Most patients don’t know this. Doctors don’t always explain it clearly. And when a woman gets pregnant three weeks after her last dose, as one Reddit user described, the damage is already done.
Beta-Carotene: The Safe Alternative
Here’s the good news: not all vitamin A is the same. Beta-carotene, the plant-based form found in carrots, sweet potatoes, and spinach, doesn’t cause birth defects. Why? Because your body only converts it to active vitamin A as needed. It can’t build up to toxic levels. Even at doses up to 180 mg per day (that’s 300,000 IU in equivalent retinol), no teratogenic effects have been observed in humans.
That’s why experts now recommend switching prenatal vitamins to those containing only beta-carotene. ConsumerLab.com found that 45% of prenatal vitamins still use retinyl palmitate. But brands like Garden of Life, New Chapter, and Nature Made now offer beta-carotene-only options. No liver damage. No risk of overdose. No fear of birth defects.
Topical Retinoids: Are They Safe?
Many women wonder: if I’m using tretinoin cream for acne, am I putting my baby at risk? The answer is mostly no. Studies show that after applying a standard amount of topical retinoid, less than 0.5 ng/mL of the drug enters the bloodstream-far below the level needed to cause harm. The FDA still recommends avoiding it during pregnancy, but not because of proven danger. It’s precaution.
Still, if you’re planning to get pregnant or think you might be, stop using retinoid creams. The skin absorbs more than you think, especially if you’re using them daily on large areas. And if you’ve been using them long-term, your body might still hold traces. Better safe than sorry.
How Much Is Too Much?
The science is clear: 10,000 IU of preformed vitamin A per day is the threshold. That’s the limit set by the WHO, ACOG, and the Institute of Medicine. But here’s the catch: you don’t need to take a supplement to hit it.
- One 3-ounce serving of beef liver = 27,000 IU
- One tablespoon of cod liver oil = 13,500 IU
- One multivitamin with retinyl palmitate = 2,500-5,000 IU
- Fortified cereal (one bowl) = 1,000-2,000 IU
Add them up. Two servings of liver a month? That’s already over 50,000 IU. One spoon of cod liver oil daily? That’s 400,000 IU a year. No wonder some women end up with babies born with heart defects-without ever taking a prescription.

What Doctors Should Be Doing
Board-certified dermatologists get it right 92% of the time. But general practitioners? Only 58%. That’s a gap. A dangerous one. A woman with severe acne might see her family doctor for a refill, not realize the risks, and keep taking isotretinoin while trying to conceive.
Doctors need to do more than hand out a pamphlet. They need to: check pregnancy status every month, confirm contraceptive use, explain the difference between beta-carotene and retinol, and warn about hidden sources like liver and fish oil. The iPLEDGE program takes 20-30 minutes per visit. That’s not a burden-it’s a requirement. And if your doctor skips it, ask why.
The Bigger Picture: Global Gaps and Future Solutions
In the U.S., we have iPLEDGE. In Europe, there’s the Pregnancy Prevention Programme. But in low-resource countries, women take isotretinoin without contraception. No testing. No counseling. No follow-up. The Lancet Global Health found that teratogenic exposure rates are 8.3 times higher in these regions.
Meanwhile, new drugs are coming. LGD-1550, a retinoid analog in Phase II trials, shows the same acne-fighting power as isotretinoin-but without the birth defect risk. That’s huge. But until it’s approved, the risk remains. And the NIH-funded Vitamin A Safety Consortium is working on better educational tools. Early results show a 32% improvement in patient understanding when they get clear, visual materials-not just a warning label.
What You Can Do Today
- Check your prenatal vitamin. Does it say “retinyl palmitate” or “vitamin A (as retinol)”? If yes, switch to one with beta-carotene.
- Stop eating liver or taking cod liver oil if you’re pregnant or trying to conceive.
- If you’re on isotretinoin, etretinate, or acitretin, use two forms of birth control. No exceptions.
- If you’re on topical retinoids, stop them before trying to get pregnant.
- Ask your doctor: “Is the vitamin A in my supplement safe for pregnancy?”
This isn’t about fear. It’s about awareness. Vitamin A isn’t the villain. Misunderstanding it is.
Can I take vitamin A while pregnant?
You can, but only in safe forms and amounts. Avoid preformed vitamin A (retinol, retinyl palmitate) in doses over 10,000 IU per day. Instead, choose supplements with beta-carotene, which your body converts only as needed. Beta-carotene is safe even at high doses. Always check your prenatal vitamin label.
Is isotretinoin (Accutane) safe during pregnancy?
No. Isotretinoin is classified as Pregnancy Category X-meaning it’s proven to cause severe birth defects. Between 20% and 35% of pregnancies exposed during the first trimester result in major malformations, including heart, brain, and facial defects. It is absolutely contraindicated during pregnancy. The iPLEDGE program exists to prevent this, and it must be followed exactly.
How long after stopping isotretinoin can I get pregnant?
For isotretinoin, the FDA recommends waiting at least one month after your last dose. But some experts suggest three months for extra safety. For acitretin, the wait is two years. For etretinate, it’s up to three years because the drug stays in fat tissue for a very long time. Never assume you’re safe just because you stopped the medication-check with your doctor.
Are topical retinoids like tretinoin cream dangerous in pregnancy?
The risk is extremely low. Studies show that topical tretinoin results in less than 0.5 ng/mL of drug in the bloodstream-far below levels known to cause harm. Still, because no exposure is 100% risk-free, most doctors advise stopping it if you’re pregnant or trying to conceive. It’s a precaution, not a proven danger.
What foods are high in dangerous vitamin A?
Beef liver is the biggest culprit-one 3-ounce serving contains 27,000 IU. Cod liver oil is next-1 tablespoon has 13,500 IU. Other sources include fortified cereals, dairy products, and some multivitamins. If you’re pregnant, avoid liver entirely and limit cod liver oil. Beta-carotene-rich foods like carrots, sweet potatoes, and spinach are safe and recommended.
Why do some prenatal vitamins still contain retinol?
Because it’s cheaper and more stable than beta-carotene. Many manufacturers haven’t updated their formulas despite decades of research showing retinol poses a risk. A 2022 ConsumerLab analysis found that 45% of prenatal vitamins still contain preformed vitamin A. Always read the label. If it says “vitamin A” without specifying beta-carotene, assume it’s retinol-and switch.
Can I get vitamin A toxicity from food alone?
Yes. Most cases of vitamin A toxicity in pregnancy come from food-not supplements. Eating liver once a week or taking cod liver oil daily can easily push intake over 30,000 IU. That’s three times the safe limit. You don’t need to be taking pills to be at risk. Real-world exposure is often from traditional diets or well-meaning advice like “eat liver for iron.” That advice can be deadly in pregnancy.
Is there a test to check vitamin A levels during pregnancy?
Not routinely. Blood tests for vitamin A exist but aren’t standard in prenatal care. Doctors rarely check them because the focus is on prevention-not measurement. The best approach is to avoid high-risk sources entirely. If you’re unsure about your intake, stop all vitamin A supplements and switch to beta-carotene. That’s the safest strategy.


Solomon Ahonsi
February 1, 2026 AT 16:40George Firican
February 3, 2026 AT 10:04Matt W
February 4, 2026 AT 12:01Anthony Massirman
February 5, 2026 AT 12:58larry keenan
February 6, 2026 AT 15:38Nick Flake
February 8, 2026 AT 14:09Akhona Myeki
February 8, 2026 AT 16:42Chinmoy Kumar
February 9, 2026 AT 08:19jay patel
February 11, 2026 AT 00:55Ansley Mayson
February 11, 2026 AT 04:15phara don
February 12, 2026 AT 14:51Hannah Gliane
February 13, 2026 AT 22:33Murarikar Satishwar
February 15, 2026 AT 01:52Bob Hynes
February 16, 2026 AT 10:41Ellie Norris
February 16, 2026 AT 22:54