Syphilis Strains in the U.S. Showing Widespread Antibiotic Resistance
The battle against sexually transmitted infections (STIs) has hit a substantial hurdle with the troubling rise of antibiotic-resistant strains of syphilis in the United States. A recent study has uncovered that nearly all isolates of the bacterium Treponema pallidum, responsible for syphilis, carry mutations making them resistant to azithromycin. The findings of the research underscore a significant public health challenge as healthcare providers are now grappling with the increased difficulty of treating this STI.
Historically, syphilis, a condition marked by stages of sores, rashes, and potentially severe systemic effects, has been treated effectively with penicillin. However, for patients allergic to penicillin, azithromycin was often employed as an alternative. The emergence of resistance to azithromycin in Treponema pallidum eliminates this crucial treatment option, complicating the management of syphilis cases significantly.
The Extent of Antibiotic Resistance
The study involved analyzing a large number of syphilis-causing bacterial samples from across the United States. Shockingly, investigators found that almost all samples contained mutations linked to azithromycin resistance. These mutations alter the bacterial ribosome, the target of azithromycin, rendering the antibiotic ineffective. This means that current treatment protocols are at risk, potentially leading to prolonged infections and increased transmission rates.
One striking aspect of the research is that it highlights the broader issue of antibiotic resistance. Bacteria have historically shown an ability to develop resistance to antibiotics over time, but the rapid and near-universal emergence of resistance in Treponema pallidum is particularly alarming. This pattern could mirror future challenges with other antibiotics and even other bacterial pathogens if not adequately addressed.
Implications for Healthcare Providers
Healthcare providers are now facing the daunting task of managing syphilis in light of these findings. The reliance on azithromycin as an alternative to penicillin for those with allergies or intolerances was a cornerstone of treatment regimens. With this option now rendered ineffective, there needs to be a reevaluation of current practices. Treatment guidelines may need to be updated to reflect the reduced utility of azithromycin, with an increased emphasis on penicillin or other alternatives that might still be effective.
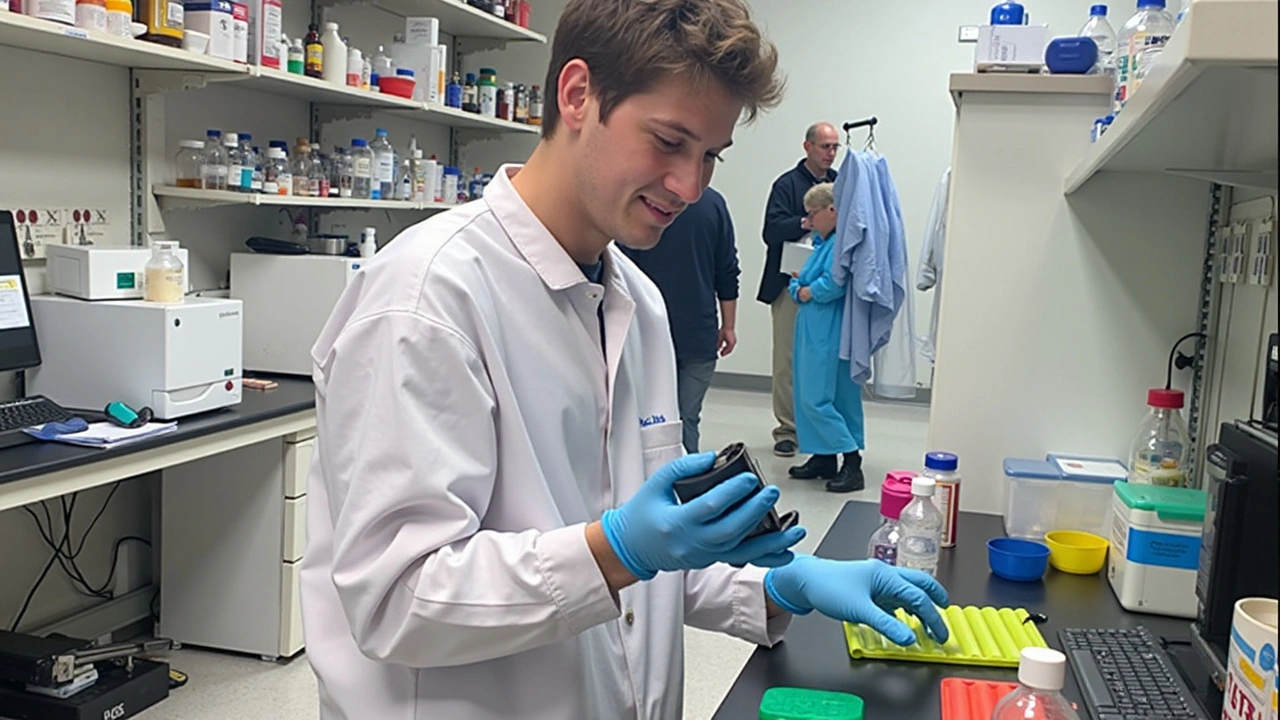
Moreover, this situation calls for enhanced diagnostic capabilities. The ability to quickly test for azithromycin resistance in patients could help tailor treatments and avoid the use of ineffective antibiotics. This development underscores the ongoing need for technological advances in medical diagnostics and the importance of timely and accurate information in combating infectious diseases.
The Way Forward: Monitoring and Research
The study’s authors stress the importance of continuous monitoring of antibiotic resistance patterns. Surveillance systems must be robust and capable of detecting changes in resistance as they occur. This ongoing vigilance is crucial to adapting treatment guidelines and ensuring the efficacy of the available therapies. It’s also vital for identifying emerging resistance trends early on, which can help in launching preemptive strategies and preserving the effectiveness of existing antibiotics.
Additionally, there is a call for intensified research into new treatment avenues. With azithromycin's efficacy now in question, researchers must investigate alternative antibiotics or combination therapies that can effectively tackle resistant strains of Treponema pallidum. There is also a pressing need to understand better the mechanisms that facilitate resistance, which can guide the development of next-generation treatments and potentially avoid the pitfalls of resistance experienced with current antibiotics.
Public Health Implications
The broader public health implications of this finding cannot be overstated. Syphilis, if not adequately treated, can progress to severe stages affecting multiple body systems and leading to long-term health complications. The risk of transmission also increases, contributing to ongoing cycles of infection within the community. Public health campaigns must now emphasize the critical importance of regular STI testing, early diagnosis, and adherence to prescribed treatments to manage and curb the spread of syphilis effectively.
Education plays a pivotal role in addressing this issue. Public awareness about the risks of untreated syphilis and the reality of antibiotic resistance can foster more responsible behaviors and support public health initiatives. Efforts to destigmatize STI testing and treatment can also encourage more individuals to seek timely medical advice and interventions.
Conclusion
In conclusion, the near-total resistance of syphilis strains in the U.S. to azithromycin presents a formidable challenge that requires immediate and coordinated action. From rethinking treatment protocols to enhancing diagnostic capabilities and intensifying research efforts, there is a multifaceted approach needed to address this growing public health threat. It is a reminder of the adaptability of bacterial pathogens and the need for continual vigilance and innovation in our efforts to combat infectious diseases. Above all, it underlines the importance of adaptive healthcare strategies in ensuring that we remain one step ahead in the ongoing battle against antibiotic resistance.


John Magnus
August 16, 2024 AT 20:15Listen up, the molecular epidemiology of Treponema pallidum has entered a post‑antibiotic epoch, and the data unequivocally demonstrate a pan‑U.S. fixation of 23S rRNA A2058G mutations that abrogate macrolide binding.
These point mutations confer a high‑level MIC escalation beyond the therapeutic window of azithromycin, rendering the drug pharmacodynamically inert.
From a pharmacokinetic perspective, azithromycin's tissue penetration is moot when the ribosomal target is structurally altered.
The selective pressure exerted by sub‑optimal dosing regimens has catalyzed clonal expansion of resistant haplotypes, a classic example of fitness‑cost neutral evolution.
Clinicians must pivot back to benzathine penicillin G as the gold standard, notwithstanding the allergic cohort.
Marc Clarke
August 21, 2024 AT 11:21Whoa, that’s some heavy science, but the takeaway is clear: we need to get back to penicillin as the mainstay and stop relying on azithro as a fallback.
angelica maria villadiego españa
August 24, 2024 AT 22:41I feel for anyone who’s allergic to penicillin – this news is scary, but it’s important to talk to your doctor about safe alternatives.
Ted Whiteman
August 27, 2024 AT 20:08Here we go again, another “crisis” in antibiotics.
Dustin Richards
August 30, 2024 AT 03:41While the situation is indeed concerning, it is essential to approach it with measured deliberation rather than alarmist rhetoric.
Vivian Yeong
September 3, 2024 AT 04:55The data is undeniable and the public health implications are serious. However, the response must be grounded in evidence‑based guidelines rather than knee‑jerk policy shifts.
suresh mishra
September 4, 2024 AT 22:35Agreed. We should focus on updated resistance testing and maintain penicillin as first‑line.
Reynolds Boone
September 9, 2024 AT 13:41This is a perfect example of why continuous surveillance is crucial; without it, we’d be blindsided by resistant strains and lose a critical treatment option.
Angelina Wong
September 11, 2024 AT 21:15Exactly, and the research community should accelerate trials for novel antimicrobial combos to stay ahead of the curve.
Anthony Burchell
September 15, 2024 AT 08:35People are overreacting; it’s just another bug in the system.
Michelle Thibodeau
September 18, 2024 AT 06:01While it may seem like a routine development, the ripple effects on community health, prenatal outcomes, and stigma around STI testing are profound and merit thoughtful intervention.
Patrick Fithen
September 22, 2024 AT 07:15One must ponder the ethical dimensions of antibiotic stewardship; a society that neglects its microbial allies invites a cascade of unintended consequences.
Michael Leaño
September 24, 2024 AT 14:48True, and staying positive while we push for better diagnostics can keep patients engaged in their own care.
Anirban Banerjee
September 28, 2024 AT 02:08Esteemed colleagues, I recommend a formal review of national treatment protocols, ensuring they reflect the latest resistance profiles with the utmost rigor.
Mansi Mehra
September 30, 2024 AT 09:41The proposal is noted; however, it lacks specificity regarding the implementation timeline and resource allocation.