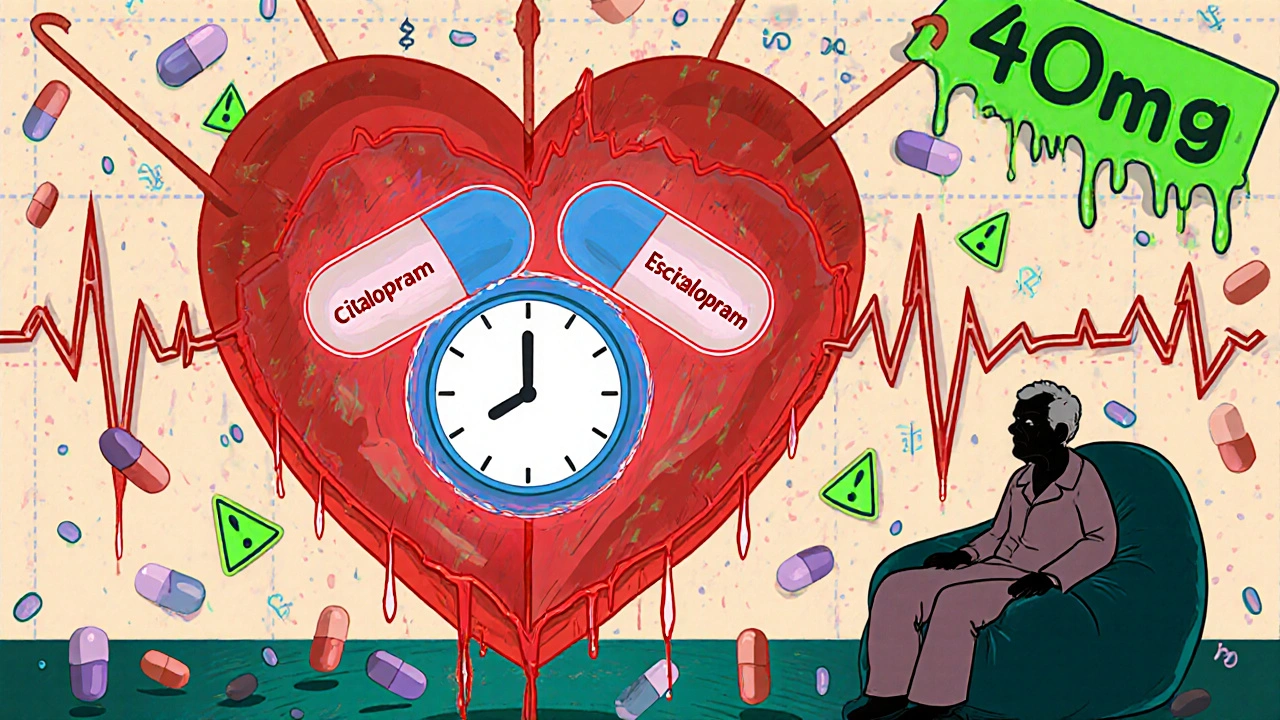
QT Interval Antidepressants: Risks, Monitoring, and Safer Choices
When you take an QT interval antidepressant, an antidepressant known to delay the heart’s electrical recovery phase, increasing the risk of irregular heartbeats. Also known as drugs that prolong the QT interval, these medications can interfere with how your heart resets after each beat—sometimes with life-threatening results. It’s not about whether the drug works for depression. It’s about whether your body can handle the hidden strain on your heart.
Not all antidepressants do this, but some of the most commonly prescribed ones do. Citalopram, a widely used SSRI that carries a clear FDA warning for QT prolongation at higher doses, is one of the biggest concerns. Escitalopram, its close relative, also carries risk, especially above 20 mg daily. Even older drugs like amitriptyline, a tricyclic antidepressant often used for nerve pain or insomnia, can stretch the QT interval. These aren’t rare edge cases—they’re in everyday prescriptions. And if you’re over 65, have heart disease, take diuretics, or are on other meds like antibiotics or antifungals, your risk jumps fast.
The danger isn’t just theoretical. A prolonged QT interval can lead to torsades de pointes, a chaotic heart rhythm that can collapse suddenly and kill within minutes. It doesn’t always come with warning signs—no chest pain, no dizziness. Sometimes, the first symptom is a cardiac arrest. That’s why doctors check your ECG before starting these drugs and again after a few weeks. Blood levels matter too. Some people metabolize these drugs slowly, letting them build up to dangerous levels without realizing it. That’s why therapeutic drug monitoring, a process that measures how much of the drug is actually in your bloodstream, isn’t just for narrow-index drugs like lithium—it’s critical here too.
And it’s not just about picking the right drug. It’s about avoiding combinations. Taking a QT-prolonging antidepressant with an antibiotic like azithromycin, or an anti-nausea pill like ondansetron, can turn a manageable risk into a crisis. Even grapefruit juice or certain herbal supplements can interfere. Your pharmacist should flag this. But you need to know to ask.
There are safer options. Sertraline, for example, has minimal effect on the QT interval. Bupropion, used for depression and smoking cessation, rarely causes this issue. But switching isn’t simple. You can’t just stop one drug and start another cold turkey. Withdrawal can trigger its own heart rhythm problems. That’s why this isn’t a DIY decision—it’s a layered conversation with your doctor, your pharmacist, and sometimes a cardiologist.
Below, you’ll find detailed comparisons of antidepressants like Anafranil and others, with clear breakdowns of cardiac risks, dosing limits, and what alternatives actually work without putting your heart on the line. You’ll see real data—not guesses—on who should avoid certain drugs, how often monitoring is needed, and what to do if you’re already on one of these medications. This isn’t fear-mongering. It’s about making sure your treatment for depression doesn’t accidentally put your heart at risk.