AFE Symptom Recognition Tool
Assess for Amniotic Fluid Embolism
This tool helps identify key symptoms of amniotic fluid embolism (AFE), a rare but life-threatening obstetric emergency. Early recognition is critical for timely intervention.
Respiratory Distress
Cardiovascular Collapse
Coagulopathy
Quick Action Checklist
For immediate response if AFE is suspected:
- Activate the obstetric emergency code immediately
- Call for rapid-response ICU staff and blood bank
- Secure airway - intubate and deliver 100% oxygen
- Begin massive transfusion protocol (1:1:1 ratio of RBC:Plasma:Platelets)
- Administer vasopressors to maintain MAP > 65 mmHg
- Monitor coagulation labs every 15-30 minutes
- Document time of onset and interventions
When a pregnant woman suddenly collapses during labor, the cause can be terrifying and hard to predict. One of the most dramatic yet uncommon triggers is amniotic fluid embolism - a condition where amniotic fluid, fetal cells, or debris enter the mother’s bloodstream and provoke a cascade of life‑threatening reactions.
What Is Amniotic Fluid Embolism?
Amniotic Fluid Embolism (often abbreviated AFE) is an obstetric emergency characterized by the rapid entry of amniotic fluid components into the maternal circulatory system. The embolic material provokes an intense inflammatory response, leading to cardiovascular collapse, severe respiratory distress, and coagulopathy known as disseminated intravascular coagulation (DIC). Though it accounts for less than 0.001% of all deliveries, its mortality rate can exceed 40% when not treated promptly.
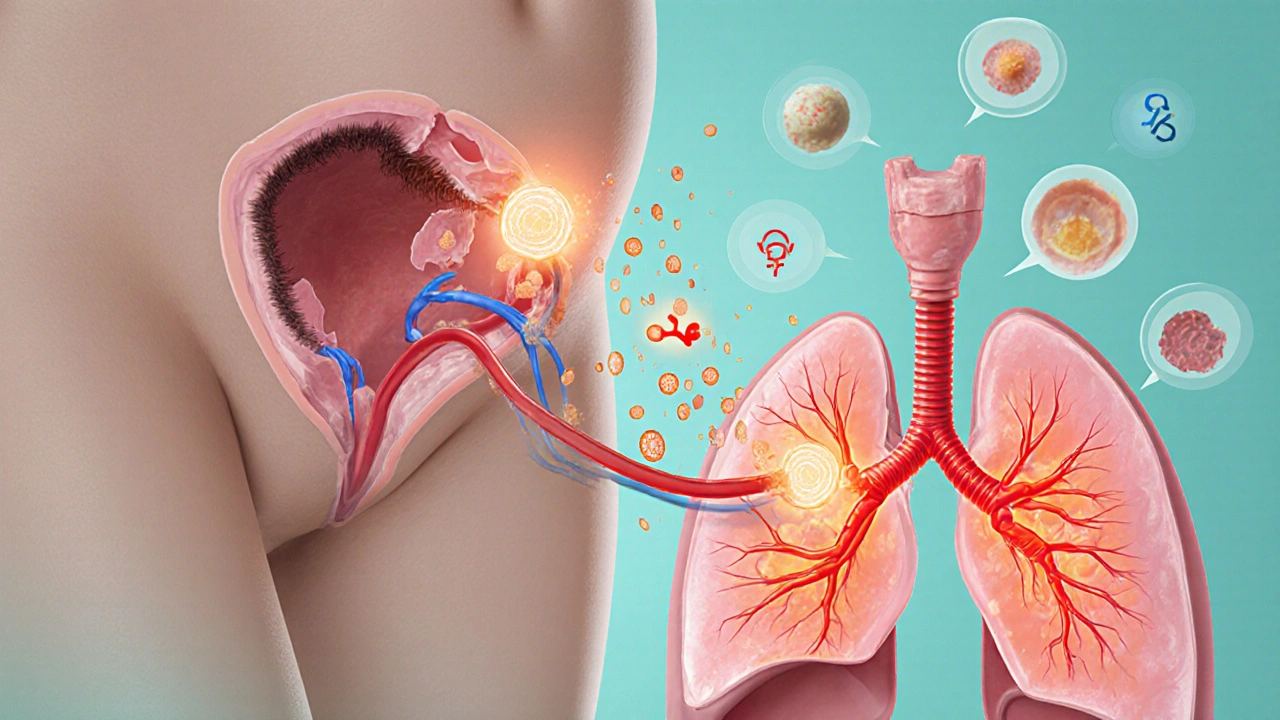
How Does It Happen? The Physiological Pathway
The exact mechanism remains partly mysterious, but clinicians typically describe three linked steps:
- Disruption of the uterine‑placental interface during labor, cesarean section, or invasive monitoring.
- Entry of amniotic fluid, fetal squamous cells, hair, or vernix into maternal veins.
- Triggering of an anaphylactoid reaction that releases histamine, cytokines, and tissue factor, which then precipitate DIC and severe vasoconstriction.
Because the offending particles travel directly to the lungs, pulmonary artery pressure spikes, causing sudden shortness of breath and hypoxia. Simultaneously, the systemic inflammatory surge can lead to myocardial depression and hemorrhagic bleeding.
Who Is at Risk?
While AFE can strike any pregnant woman, several risk factors appear more frequently in reported cases:
- Multiparity (having delivered several children)
- Advanced maternal age (>35 years)
- Placental abnormalities such as previa or abruption
- Instrumental delivery or emergency cesarean delivery
- Use of uterine stimulants (oxytocin) or amniotic rupture before full labor
It’s crucial to remember that these are trends, not guarantees - AFE can also occur without any identifiable risk.
Recognising the Signs: AFE Symptoms in Real Time
Because the condition evolves within minutes, rapid recognition saves lives. The classic triad includes:
- Respiratory distress: sudden coughing, choking, or a feeling of suffocation.
- Cardiovascular collapse: abrupt drop in blood pressure, tachycardia followed by bradycardia, and loss of consciousness.
- Coagulopathy: profuse bleeding from IV sites, uterine atony, or bruising that can’t be stopped.
Other warning signs may surface first, such as a sharp chest pain, a sense of impending doom, or a rapid rise in heart rate that quickly turns into a flatline. In practice, clinicians often describe the scenario as a “perfect storm” of respiratory, cardiac, and bleeding emergencies occurring almost simultaneously.
Diagnosis: How Medical Teams Confirm AFE
There is no single laboratory test that nails the diagnosis, so physicians rely on a combination of clinical observation and exclusion of other causes (e.g., pulmonary embolism, anaphylaxis). Common investigations include:
- Arterial blood gas showing severe hypoxia and metabolic acidosis.
- Complete blood count revealing sudden drop in platelets.
- Coagulation profile (PT, aPTT, fibrinogen) indicating DIC.
- Echocardiography demonstrating right‑ventricular strain.
- Fetal squamous cells found in maternal pulmonary or peripheral blood samples - a finding that supports but does not prove AFE.
Because time is of the essence, treatment usually begins before all results return.
Treatment: The Immediate Management Protocol
Managing AFE is about buying minutes while the body fights the cascade. The steps follow a “ABC” (Airway, Breathing, Circulation) approach, layered with aggressive correction of coagulopathy.
- Airway and oxygenation: rapid intubation, 100% oxygen, and ventilation support. In many cases, clinicians resort to high‑frequency oscillatory ventilation or extracorporeal membrane oxygenation (ECMO) if conventional methods fail.
- Circulatory support: large‑bore IVs, crystalloid boluses, and promptly administered vasopressors (e.g., norepinephrine) to sustain blood pressure.
- Blood product administration: a massive transfusion protocol delivering packed red cells, fresh frozen plasma, platelets, and cryoprecipitate in ratios that aim to reverse DIC.
- Uterine management: uterotonics (oxytocin, methylergometrine) and uterine massage to reduce bleeding.
- Critical care monitoring: transfer to an ICU for continuous hemodynamic, respiratory, and coagulation surveillance.
Experimental therapies such as recombinant activated factor VII or corticosteroids have been tried in isolated cases, but robust evidence is lacking.
Outcomes and Long‑Term Follow‑Up
Survival rates have improved modestly over the last decade, largely due to faster recognition and standardized massive‑transfusion protocols. Yet, approximately 30-40% of survivors experience neurological sequelae, renal impairment, or chronic pulmonary issues. Ongoing follow‑up includes:
- Neuro‑cognitive assessment at 6‑month intervals.
- Renal function labs (creatinine, GFR) for the first year.
- Psychological counseling for both mother and partner, given the traumatic nature of the event.
Future pregnancies carry a slightly higher risk of recurrence - estimates range from 1 in 10,000 to 1 in 20,000 deliveries - so pre‑conception counseling and a detailed delivery plan are essential.

Prevention: Can AFE Be Avoided?
Because the exact trigger isn’t fully understood, primary prevention is limited. Nonetheless, clinicians can lower the odds by:
- Minimising invasive procedures (e.g., amniocentesis, uterine instrumentation) unless medically necessary.
- Managing labor progress carefully, avoiding forceful uterine massage or excessive oxytocin dosing.
- Promptly treating placental complications such as previa or abruptio.
- Ensuring rapid access to blood products and a designated obstetric emergency team in high‑risk centers.
Patients should be educated about warning signs so they can alert staff immediately if they feel sudden breathlessness or chest discomfort during labor.
Comparing AFE with Other Obstetric Emergencies
| Feature | Amniotic Fluid Embolism | Postpartum Hemorrhage | Uterine Rupture |
|---|---|---|---|
| Incidence | ~1 per 40,000 deliveries | ~1‑5 per 1,000 deliveries | ~1 per 5,000‑10,000 deliveries |
| Onset | Sudden, during labor or shortly after delivery | Within 24hrs post‑delivery, often gradual | Often during active labor, especially with scarred uterus |
| Primary Symptoms | Respiratory distress, cardiovascular collapse, DIC | Profuse vaginal bleeding, uterine atony | Severe abdominal pain, fetal distress, loss of fetal station |
| Critical Treatment | Airway support, massive transfusion, ECMO if needed | Uterotonics, blood products, surgical intervention | Immediate laparotomy, hysterectomy if uncontrolled |
| Mortality Rate | 30‑45% | ~1‑5% | ~5‑10% |
What to Do If You Suspect AFE: A Quick Action Checklist
- Activate the obstetric emergency code immediately.
- Call for rapid‑response ICU staff and blood bank.
- Secure airway - intubate and deliver 100% oxygen.
- Begin massive transfusion protocol (1:1:1 ratio of RBC:Plasma:Platelets).
- Administer vasopressors to maintain MAP >65mmHg.
- Monitor coagulation labs every 15‑30minutes; replace fibrinogen aggressively.
- Document time of onset, interventions, and maternal vitals for future review.
Having this checklist posted in delivery suites has been shown to shave critical minutes off the response time.
Frequently Asked Questions
How common is amniotic fluid embolism?
It occurs in roughly 1 in 40,000 to 1 in 80,000 deliveries, making it one of the rarest obstetric emergencies.
Can AFE happen after a C‑section?
Yes. In fact, about 30% of reported cases occur during or shortly after a cesarean delivery, often linked to uterine incision and rapid fluid shifts.
What are the chances of surviving AFE?
Survival has improved to about 60‑70% in well‑equipped centers with rapid massive‑transfusion protocols and critical‑care support.
Will I be able to have another pregnancy after AFE?
Future pregnancies are possible but carry a slightly higher recurrence risk. Detailed pre‑conception counseling and a delivery plan are essential for safety.
Are there any preventive measures I can take?
While AFE cannot be fully prevented, minimizing invasive procedures, careful labor management, and early treatment of placental problems can reduce overall risk.
Amniotic fluid embolism may be rare, but its impact is profound. Knowing the signs, having a rapid response plan, and understanding the treatment pathway can mean the difference between life and death for both mother and baby.


kevin tarp
October 12, 2025 AT 00:59Just a quick note – the abbreviation for amniotic fluid embolism is AFE, not "AF" as seen in the second paragraph. Consistency helps readers keep track.
ravi kumar
October 14, 2025 AT 08:32While we’re nitpicking, let’s not forget that many nations lack the resources to even recognize AFE, let alone run massive‑transfusion protocols. The article’s focus on high‑tech interventions feels a bit US‑centric. A broader perspective on low‑resource settings would be more inclusive. Moreover, the risk factors listed don’t mention socioeconomic status, which is a glaring omission. We need to highlight global disparities, not just clinical minutiae.
SandraAnn Clark
October 16, 2025 AT 16:05Life is fragile; AFE reminds us how quickly the ordinary can become extraordinary.
Rex Wang
October 18, 2025 AT 23:39Wow, this is intense!!! I can’t imagine being in that room, heart racing, trying to keep everything together. The checklist looks solid, and the emphasis on rapid response is exactly what you need. The tone is respectful yet urgent-nice balance. ❤️
mark Lapardin
October 21, 2025 AT 07:12Agreed, the checklist is a lifesaver. Adding a quick reference for "dose‑dependent vasopressor titration" could further streamline the protocol. Also, consider a reminder to verify blood type and cross‑match early; it saves precious seconds.
Barry Singleton
October 23, 2025 AT 14:45The article nails the pathophysiology, but it could benefit from a brief note on the role of complement activation. That mechanistic detail is often overlooked in bedside guides, yet it underpins the cascade leading to DIC.
Javier Garcia
October 25, 2025 AT 22:19Interesting read-does anyone know if ECMO is available in community hospitals?
christian quituisaca
October 28, 2025 AT 04:52Great job breaking down such a terrifying condition into digestible steps! 🌟 The use of bold headings and the tri‑color alerts really help the eye. For anyone new to obstetrics, this is a golden road‑map. Keep spreading this knowledge; it could save lives.
Donnella Creppel
October 30, 2025 AT 12:25Well, *sure*, but why does the article *never* mention the emotional toll on the family? It's not just about labs and codes; it's about humans. Also, the term "rapid‑response" sounds like a buzzword-maybe "critical‑response" would be more apt??
Jarod Wooden
November 1, 2025 AT 19:59Amniotic fluid embolism (AFE) epitomizes the intersection of obstetric vigilance and critical care acumen. First, the abrupt incursion of fetal debris-squamous cells, vernix caseosa, mucin-into the maternal pulmonary vasculature triggers an anaphylactoid surge. Histamine, tryptase, and complement fragments cascade, precipitating a rapid rise in pulmonary artery pressures and right‑ventricular strain. Simultaneously, the endothelial insult unleashes tissue factor, igniting disseminated intravascular coagulation (DIC). This coagulopathy manifests as profuse bleeding from IV sites, uterine atony, and refractory hemorrhage. Clinically, the patient presents with a triad: sudden respiratory distress, cardiovascular collapse, and coagulopathy, often within seconds of a triggering event such as uterine rupture or vigorous fundal massage. Early recognition hinges on appreciating that the onset is precipitous-there is no slow prodrome. Diagnostic work‑up is essentially exclusionary: arterial blood gas shows severe hypoxemia, coagulation panels reveal consumptive coagulopathy, and echocardiography may demonstrate right‑heart dilation. Fetal squamous cells in peripheral blood, while supportive, are not pathognomonic. Management follows an ABC approach, but the waters are murky; airway protection with rapid sequence intubation is mandatory, and oxygenation may require high‑frequency oscillatory ventilation or ECMO in refractory cases. Hemodynamic support mandates large‑bore intravenous access, crystalloid boluses, and vasopressors-norepinephrine being first‑line to maintain a MAP >65 mmHg. Massive transfusion protocols must be activated instantly, delivering packed red cells, fresh frozen plasma, platelets, and cryoprecipitate in a 1:1:1:1 ratio to stave off exsanguination. Uterotonic agents such as oxytocin, methylergometrine, and carboprost are employed to curb uterine bleeding, and surgical measures (uterine artery ligation, hysterectomy) may become inevitable. Post‑resuscitation, patients require intensive care monitoring for multiorgan dysfunction, with serial labs tracking coagulation status, renal function, and neurologic integrity. Survivors often endure lingering sequelae-cognitive deficits, chronic pulmonary hypertension, or renal impairment-necessitating long‑term follow‑up. Future pregnancies carry a modestly elevated recurrence risk; pre‑conception counseling and delivery planning in tertiary centers with ready blood products are prudent. Ultimately, AFE remains a rare yet devastating obstetric emergency, where rapid interdisciplinary response can mean the difference between life and death.
lee charlie
November 4, 2025 AT 03:32Thanks for the thorough breakdown-it's reassuring to know that such protocols exist. I hope more hospitals adopt these checklists.
Greg DiMedio
November 6, 2025 AT 11:05Another “must‑read” post about a condition nobody will ever see, right?
Badal Patel
November 8, 2025 AT 18:39Esteemed colleagues, permit me to declare that the exposition upon amniotic fluid embolism, whilst exhaustive, lacks the requisite gravitas befitting such a cataclysmic event; one must, with all due solemnity, underscore the inevitability of mortality should the protocol be neglected-therefore, let us proceed with utmost dedication.
KIRAN nadarla
November 11, 2025 AT 02:12Good article, but the grammar in the third paragraph is off-"are" should be "is" when referring to the "triad". Minor point, yet precision matters in medical literature.
Kara Guilbert
November 12, 2025 AT 23:59We mustnt forget the moral duty to protect mothers-any neglect is unacceptable.