Depigmentation Treatment Decision Helper
Benoquin Cream is a topical formulation of monobenzone (20mg/g) used to induce uniform depigmentation in patients with extensive vitiligo. It works by permanently destroying melanocytes, creating a light‑stable skin tone that matches surrounding depigmented areas. Benoquin is the only FDA‑approved drug specifically labeled for therapeutic depigmentation, though its use is regulated and requires specialist supervision.
TL;DR - Quick Takeaways
- Monobenzone offers permanent, uniform skin whitening but carries a higher risk of irritation and requires lifelong sun protection.
- Hydroquinone, kojic acid, azelaic acid and mequinol are reversible lightening agents; they act on melanin synthesis rather than melanocyte destruction.
- Procedural options-laser depigmentation, cryotherapy, and surgical excision-provide targeted results but may need multiple sessions and carry scarring risks.
- Choosing the right approach depends on extent of vitiligo, skin type, budget, and tolerance for side‑effects.
- Always consult a dermatologist before starting any depigmentation regimen.
How Benoquin Cream Works
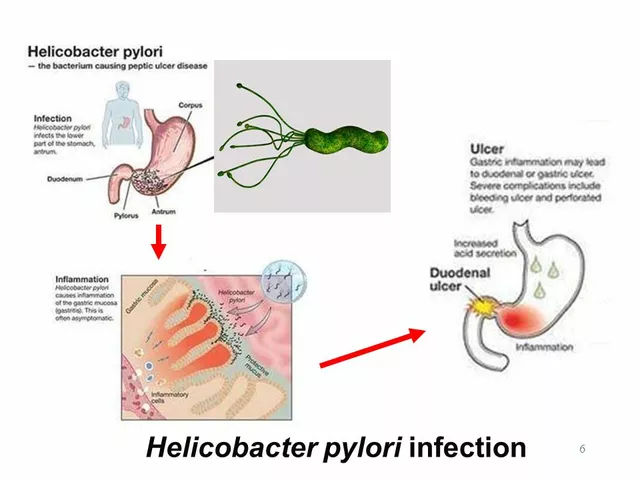
Monobenzone is a phenolic compound that binds irreversibly to tyrosinase, the key enzyme in melanin production. By disabling tyrosinase, melanocytes can no longer synthesize pigment, and over weeks they undergo apoptosis. The result is a permanent loss of colour in treated patches, typically visible after 2-3months of twice‑daily application.
Because it destroys melanocytes, Benoquin is not a cosmetic lightener; it is a medical therapy for patients who have lost most of their pigmented skin and prefer a uniform appearance. The treatment schedule usually starts with a small test area, progresses to full‑body coverage, and may last up to a year depending on skin response.
Key Attributes of Benoquin Cream
- Concentration: 20mg/g (2%) monobenzone.
- Onset: Visible depigmentation within 6-8weeks; full effect by 6-12months.
- Regulatory status: FDA‑approved for therapeutic depigmentation; available in limited markets under prescription.
- Side‑effects: Local irritation, erythema, pruritus; rare cases of vitiligo‑like spreading beyond treated zones.
- Sun protection: Mandatory lifelong SPF30+ to prevent sunburn on depigmented skin.
Common Chemical Alternatives
For patients who need a reversible or milder approach, several topical agents are widely used. Below are the most referenced alternatives, each with its own mechanism and risk profile.
Hydroquinone is a phenolic skin‑lightening agent (typically 2-4% concentration) that inhibits tyrosinase activity, slowing melanin synthesis. It is the gold standard for hyperpigmentation but is not approved for permanent depigmentation.
Kojic Acid is a fungal metabolite used in concentrations of 1-2% that chelates copper at the active site of tyrosinase, thereby reducing pigment formation.
Azelaic Acid (15-20% gel) works by inhibiting mitochondrial oxidation in melanocytes and also has mild anti‑inflammatory properties, making it useful for post‑inflammatory hyperpigmentation.
Mequinol (4‑hydroxyanisole, 2% cream) combines with tretinoin to block melanin synthesis more potently than hydroquinone alone, often used for melasma.
Procedural Alternatives
When topical creams are insufficient or the patient prefers a faster result, clinicians may turn to physical methods.
Laser Depigmentation (commonly Q‑switch Nd:YAG) emits high‑energy pulses that fragment melanin granules, which are then cleared by the immune system. Multiple sessions are typical, and results can be long‑lasting but not always permanent.
Cryotherapy applies liquid nitrogen to targeted pigmented lesions, causing melanocyte destruction through freeze‑induced cell death. It’s quick but may cause hypopigmented scars.
Surgical Excision removes localized hyperpigmented patches (e.g., nevus) with a scalpel or laser ablation, followed by grafting or primary closure. Best for small, well‑defined lesions.

Comparison Table - Benoquin vs. Common Alternatives
| Agent | Mechanism | Typical Concentration | Onset of Action | Reversibility | Common Side‑effects |
|---|---|---|---|---|---|
| Benoquin (Monobenzone) | Irreversible melanocyte destruction | 20mg/g (2%) | 6-12months for full effect | Permanent | Irritation, erythema, sunburn risk |
| Hydroquinone | Tyrosinase inhibition | 2-4% | 2-4weeks | Reversible (discontinues within months) | Contact dermatitis, ochronosis (rare) |
| Kojic Acid | Copper chelation of tyrosinase | 1-2% | 4-6weeks | Reversible | Allergic dermatitis, sensitisation |
| Azelaic Acid | Inhibits melanin synthesis & inflammation | 15-20% | 6-8weeks | Reversible | Burning, dryness |
| Mequinol | Melanin synthesis blockade (with tretinoin) | 2% | 4-6weeks | Reversible | Redness, peeling |
| Laser Depigmentation | Photothermolysis of melanin granules | - | Immediate pigment reduction | Long‑lasting but not permanent | Hypopigmentation, scarring |
| Cryotherapy | Freeze‑induced melanocyte death | - | Immediate to weeks | Often permanent in treated spot | Blistering, hypopigmented scars |
| Surgical Excision | Physical removal of pigmented tissue | - | Immediate | Permanent (if fully excised) | Scarring, infection |
Choosing the Right Option - Decision Criteria
- Extent of Vitiligo: Whole‑body depigmentation (Benoquin) vs. focal lesions (laser, cryotherapy, surgery).
- Desired Permanence: Permanent melanocyte loss (monobenzone, surgical) vs. reversible agents (hydroquinone, kojic acid).
- Skin Type & Colour: Darker Fitzpatrick IV-VI skin is more prone to post‑inflammatory hyperpigmentation after laser; chemical agents may be safer.
- Budget & Access: Prescription monobenzone can be expensive and limited to specialist clinics; over‑the‑counter agents (hydroquinone, azelaic acid) are cheaper.
- Side‑effect Tolerance: If irritation is a concern, start with low‑strength azelaic acid; if you can manage strict sun protection, Benoquin is viable.
Putting these factors into a simple matrix helps patients and clinicians visualise the trade‑offs. For example, a patient with extensive vitiligo who wants a uniform colour and is willing to commit to lifelong photoprotection may find Benoquin the most logical choice, while a cosmetically‑sensitive individual with isolated hyperpigmentation might prefer a short‑term hydroquinone regimen.
Managing Side‑effects & After‑care
Regardless of the chosen method, proper after‑care reduces complications.
- Sun protection: SPF30+ broad‑spectrum clothing is mandatory after monobenzone or laser, as depigmented skin burns easily.
- Moisturisation: Petrolatum‑based ointments soothe irritation from hydroquinone, kojic acid, or azelaic acid.
- Patch testing: Always test a new chemical agent on a 2cm² area for 48hours to gauge sensitisation.
- Follow‑up visits: Schedule dermatology appointments every 4-6weeks for monobenzone to monitor spread and adjust dosage.
Real‑World Scenarios
Case 1 - Full‑body depigmentation: Sarah, 34, had 85% body surface involvement with vitiligo. After failed topical lighteners, her dermatologist prescribed Benoquin. Over 10months, her skin tone equalised, and she now uses SPF50 sunscreen daily. She reports mild itching during the first 3months, managed with hydrating cream.
Case 2 - Localised melasma: Raj, 28, presented with facial melasma. He opted for a combo of hydroquinone 4% and azelaic acid 15% gel under physician guidance. After 12weeks, pigment lightened by 60%, with no rebound after tapering.
Case 3 - Post‑inflammatory hyperpigmentation after acne: Maya, 22, used kojic acid serum twice daily. Within 8weeks, her dark spots faded, but she experienced occasional irritation, which resolved after adding a barrier cream.
Bottom Line
If you need a permanent, uniform skin colour across large areas, monobenzone alternatives such as Benoquin remain the cornerstone, albeit with a commitment to strict sun protection and medical supervision. For reversible or focal concerns, chemical agents like hydroquinone, kojic acid, azelaic acid, and procedural methods such as laser or cryotherapy provide flexibility but may require multiple sessions or carry different risk profiles.
The decision ultimately balances extent of pigment loss, desire for permanence, tolerance for side‑effects, and practical considerations like cost and access. Consulting a board‑certified dermatologist ensures the chosen path aligns with your skin type and health goals.
Frequently Asked Questions
Is Benoquin Cream safe for long‑term use?
Benoquin is considered safe when prescribed by a dermatologist and used as directed. Long‑term safety hinges on diligent sun protection and regular skin checks to catch any adverse reactions early.
Can I combine monobenzone with other skin‑lightening agents?
Combining monobenzone with other agents is generally discouraged because it may increase irritation and complicate monitoring of pigment loss. If additional lightening is needed, discuss a staged approach with your doctor.
How does laser depigmentation differ from monobenzone?
Laser treatment physically breaks down melanin and removes it, offering quicker visible results but often requires multiple sessions and may not be permanent. Monobenzone chemically eliminates melanocytes, leading to permanent depigmentation but over a longer timeline.
Are there natural alternatives to monobenzone?
Natural extracts like licorice root, niacinamide, and arbutin can modestly brighten skin, but they do not achieve the depth of depigmentation required for extensive vitiligo. They are better suited for mild hyperpigmentation.
What is the cost comparison between Benoquin and other treatments?
Benoquin can cost up to $300-$500 per month in many countries due to its prescription status. Over‑the‑counter agents like hydroquinone or azelaic acid range from $20-$70 for a standard tube. Laser sessions can run $150-$400 each, often needing 3-5 visits.


Shane matthews
September 25, 2025 AT 06:01Monobenzone definitely isn’t for everyone.
Rushikesh Mhetre
September 28, 2025 AT 17:23Wow this guide is a goldmine!!! It breaks down every option so clearly, you can actually compare them side‑by‑side!!! The interactive tool is super handy, just plug in your numbers and boom-you get a recommendation!!! I love how it highlights the need for lifelong sunscreen with Benoquin-that’s a game‑changer!!!
Sharath Babu Srinivas
October 2, 2025 AT 04:43Great summary 😊. The table makes the differences pop, especially the permanence column. I appreciate the note about monitoring for spread beyond treated zones-safety first! 👍
Halid A.
October 5, 2025 AT 16:05The inclusion of post‑treatment care is essential; many patients overlook sunscreen and moisturisation. Your emphasis on regular dermatologist visits aligns with best practice. Well‑structured and thorough.
Brandon Burt
October 9, 2025 AT 03:31Reading through this piece feels like taking a deep dive into the entire depigmentation universe, and honestly, it’s impressive how comprehensively everything is covered! First, the distinction between irreversible melanocyte destruction and reversible tyrosinase inhibition is crystal clear, which is crucial for anyone weighing options. Second, the side‑effect profiles are laid out with no sugar‑coating, reminding us that every powerful tool comes with trade‑offs! Third, the cost analysis is blunt yet necessary-knowing that Benoquin can run into the hundreds per month prevents surprise budget shocks. Fourth, the procedural alternatives like laser and cryotherapy are presented not as after‑thoughts but as viable paths for focal lesions, expanding the decision matrix beyond creams alone. Fifth, the real‑world case studies ground the data in lived experience, showing both successes and manageable setbacks. Sixth, the emphasis on lifelong sun protection after monobenzone use cannot be overstated; it’s a non‑negotiable safety net. Seventh, the guidance to patch‑test new agents for 48 hours demonstrates a proactive approach to irritation. Eighth, the timeline expectations-6‑12 months for full effect-set realistic patient expectations and help avoid premature discontinuation. Ninth, the discussion of combination therapies wisely cautions against indiscriminate mixing, preserving treatment clarity. Tenth, the FAQ section anticipates common concerns, saving readers from endless internet searches. Eleventh, the layout’s interactive calculator is a practical tool that translates abstract criteria into personalized advice. Twelfth, the table’s side‑by‑side comparison of mechanisms, concentrations, and reversibility reads like a quick‑reference cheat sheet. Thirteenth, the article repeatedly stresses consulting a board‑certified dermatologist, reinforcing professional oversight. Fourteenth, the inclusion of both chemical and procedural options respects the diversity of patient preferences. Fifteenth, the narrative maintains a balanced tone-neither hyping Benoquin nor disparaging other methods-allowing readers to make informed choices. Lastly, the concluding “Bottom Line” neatly encapsulates the hierarchy of considerations, making the whole thing feel like a well‑orchestrated guide rather than a disjointed list. Overall, this is a standout resource for anyone navigating the complex world of depigmentation treatments!
Gloria Reyes Najera
October 12, 2025 AT 15:00Benoquin is just a pricey fad for americans who cant afford real skincare.
Gauri Omar
October 16, 2025 AT 02:28Wow, the drama of losing pigment forever is like watching a tragic play, but the science behind it is fascinating! If you’re brave enough to go full‑on, Benoquin is the starring role-dark, permanent, and demanding. Yet, the supporting cast of hydroquinone, kojic acid, and lasers can steal the show for those who prefer a cameo instead of a lead. Remember, every protagonist needs a good script, and in this case the script is lifelong SPF and dermatologist check‑ups.
Willy garcia
October 19, 2025 AT 13:56Good to see the emphasis on sunscreen-essential for anyone using Benoquin.
zaza oglu
October 23, 2025 AT 01:26Super helpful guide! 🎨 It paints the whole picture with bright, vivid detail; you can actually see which option shines brightest for your skin type and budget.
Vaibhav Sai
October 26, 2025 AT 11:58Loving the clear breakdown! The colorful table makes it easy to pick a path-whether you want a quick laser zap or the steady march of monobenzone.
Lindy Swanson
October 29, 2025 AT 23:30Honestly, I think most people overcomplicate this-just pick whatever feels right.
Amit Kumar
November 2, 2025 AT 11:01Great info! 🙌 Keep it coming, and thanks for the emojis 😊
Crystal Heim
November 5, 2025 AT 22:35The guide is solid, but don’t forget to watch for side‑effects.
Sruthi V Nair
November 9, 2025 AT 10:10Philosophically speaking, choosing a permanent skin change raises questions about identity and acceptance-worth pondering alongside the clinical data.
Mustapha Mustapha
November 12, 2025 AT 21:46Nice work on the long‑form analysis; the step‑by‑step timeline really helps set realistic expectations for patients.
Ben Muncie
November 16, 2025 AT 09:25While enthusiasm is great, the risks of lifelong sunburn with monobenzone shouldn’t be downplayed.
kevin tarp
November 19, 2025 AT 21:05Correction: "lifelong" should be hyphenated in that context; also, "sunburn" is a noun, not a verb.
ravi kumar
November 23, 2025 AT 08:46American consumers love their pricey creams-Benoquin is just another export to cash in on their insecurities.
SandraAnn Clark
November 26, 2025 AT 20:30Seems like a lot of info for people who just want a quick fix.
Rex Wang
November 30, 2025 AT 08:15Appreciate the balanced tone; the reminder to consult a dermatologist is especially important.