When your child misses a dose of medicine, panic is normal. But doubling up? That’s dangerous. Kids aren’t small adults. Their bodies process drugs differently, and even a small mistake can lead to serious harm. According to the American Academy of Pediatrics, medication errors cause nearly 1 in 10 preventable adverse events in hospitalized children-and dosing mistakes make up over a third of those errors. The good news? With clear rules, you can avoid the most common traps.
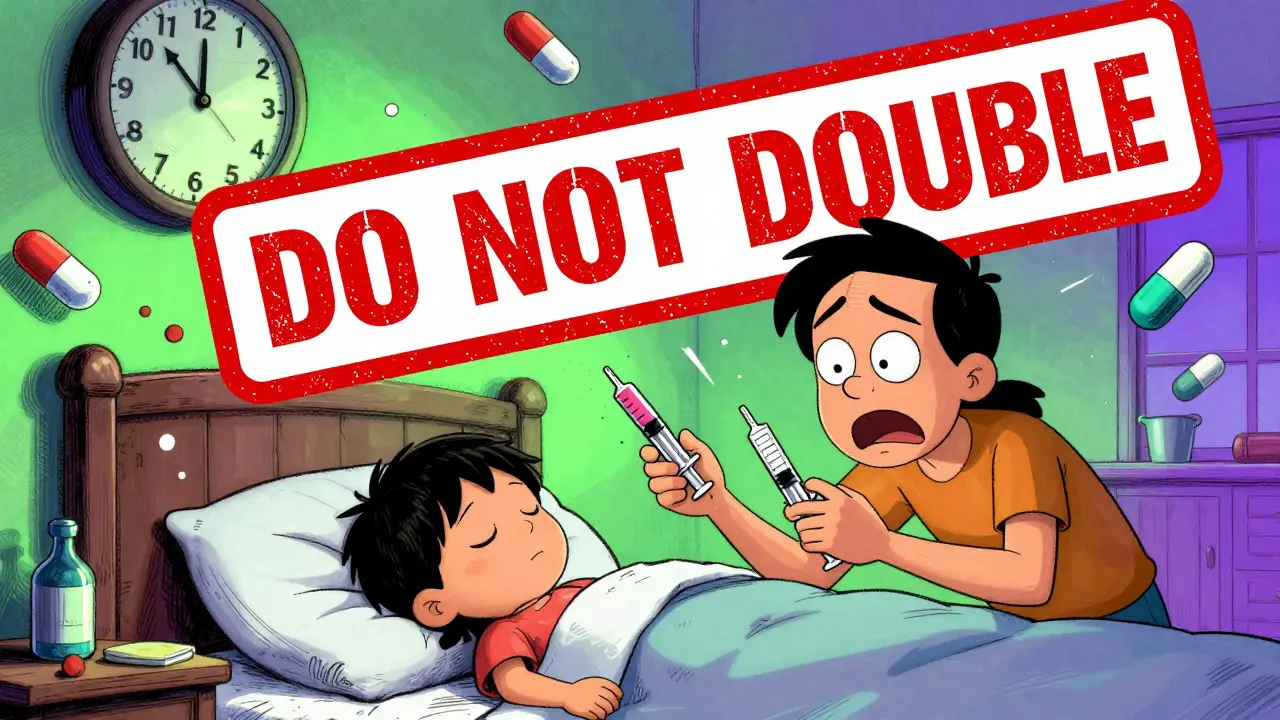
Never Double the Dose
This is the golden rule. Ever. If your child missed a dose and you’re tempted to give two pills or double the liquid to make up for it, stop. Never double the dose. Children’s livers and kidneys are still developing. They can’t flush out extra medicine like adults can. Dr. Sarah Verbiest’s 2023 review found that doubling doses increases the risk of severe reactions in kids under 12 by 278%. For medications like morphine, lorazepam, or antibiotics, that extra amount can cause breathing problems, low blood pressure, or seizures.One parent on Reddit admitted they doubled a dose of amoxicillin because they didn’t want their child to fall behind. The result? Vomiting, drowsiness, and a trip to the ER. It wasn’t an overdose-but it was close enough to scare them for life. Stick to the plan. Skip the missed dose. Move on.
Time-Based Rules: What to Do Based on Frequency
There’s no one-size-fits-all answer. The clock matters. How late you are determines whether you give the dose or skip it. Here’s what major children’s hospitals recommend:- Once daily: Give it if you’re less than 12 hours late. If it’s been more than 12 hours, skip it. Don’t give it the next day early to catch up.
- Twice daily (every 12 hours): Give it if you’re less than 6 hours late. If it’s been 6+ hours, skip it. The next dose should be at the regular time.
- Three times daily (every 8 hours): Give it if you’re less than 3 hours late. Beyond that, skip it.
- Four times daily (every 6 hours): Give it only if you’re less than 2 hours late. After that, skip it.
- Every 2-4 hours (like pain meds or seizure meds): If you’re more than 2 hours late, skip it. These meds are timed tightly-delaying too long can trigger symptoms.
These thresholds aren’t arbitrary. They’re based on how long the drug stays active in the body. Giving it too late and then too soon creates dangerous spikes in blood levels. Children’s Wisconsin and Cincinnati Children’s Hospital both use these same time windows because they’ve been tested in real clinical settings.
Special Cases: High-Risk Medications
Some meds need a different approach. If your child takes chemotherapy, immunosuppressants, or seizure medications like phenytoin, missing even one dose can affect treatment. For these, call the doctor or pharmacist immediately. Don’t guess. Don’t wait. These are classified as “red” category drugs by the National Patient Safety Agency-meaning they’re high-risk and often lack clear instructions on the label. In fact, 25% of high-risk pediatric medications have no missed-dose guidance at all on their packaging. That’s not your fault. It’s a system failure. So you take control: call ahead.For antibiotics like amoxicillin or azithromycin, skipping a dose once usually won’t ruin the course-but consistency matters. If your child misses two doses in a row, check in. Incomplete antibiotic courses can lead to resistant infections. But again: never double up.
How to Avoid Missed Doses in the First Place
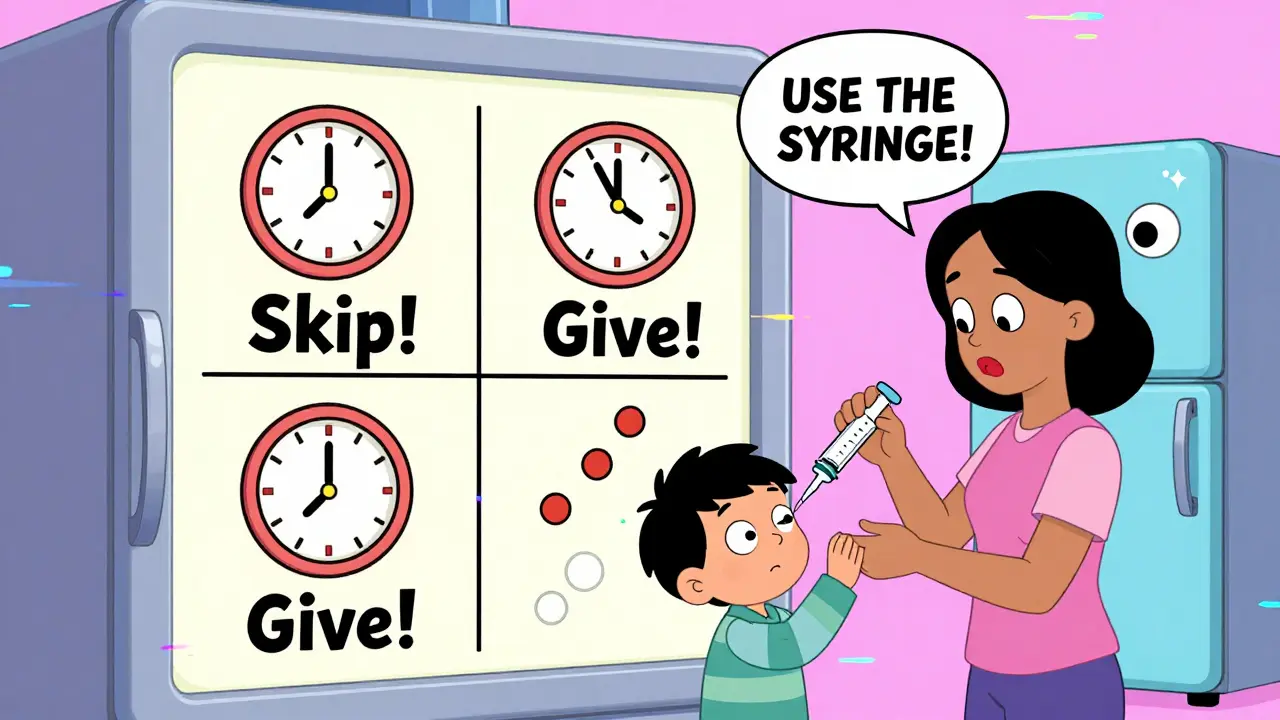
Prevention beats correction. Here’s how to reduce the chance of missing doses:- Use an oral syringe, not a spoon. Household teaspoons vary wildly. The FDA says 22% of dosing errors come from spoon confusion. A plastic syringe with clear markings cuts that risk by more than half.
- Set phone alarms. Label them clearly: “Emma - Amoxicillin 8am.” Don’t rely on memory. Even parents of healthy kids miss doses-37% of them, according to one study.
- Use color-coded charts. Boston Children’s Hospital found that color-coded daily schedules reduced missed doses by 44% for kids with complex needs. Red for morning, blue for afternoon, green for night. Simple. Visual. Hard to mess up.
- Teach-back method. Before leaving the hospital, ask your nurse: “Can you show me how to give this?” Then have your partner or another caregiver demonstrate it back to you. Cincinnati Children’s cut errors by 37% using this simple trick.
- Keep a log. A small notebook or app where you check off each dose helps you spot patterns. Did you miss the 3 p.m. dose three days in a row? Maybe your schedule doesn’t match your work hours. Adjust the timing with your doctor’s approval.
What About Liquid Medicines and Weight-Based Dosing?
Many pediatric meds are dosed by weight-not age. If your child’s weight changes, the dose should change too. But here’s the problem: 74% of morphine and 73% of lorazepam dosing errors in emergency settings come from guessing weight based on age. That’s risky. A 2-year-old weighing 10 kg needs a very different dose than one weighing 16 kg, even if they’re both “about 2 years old.”Ask your provider for your child’s exact weight in kilograms and keep it written down. Use a scale that measures in kg. Many hospitals now use length-based resuscitation tapes (like the Broselow tape) to estimate weight quickly during emergencies. These reduce weight estimation errors by 42%. If your child’s doctor hasn’t given you a weight-based chart, ask for one.

What If You’re Still Unsure?
If you’re confused-don’t guess. Don’t rely on the label. Many patient information leaflets don’t even include missed-dose instructions. A 2021 review found that 25% of high-risk pediatric meds had zero guidance on what to do if a dose was missed.Call your pediatrician’s office. Most have a nurse line open after hours. If it’s after hours and you’re worried about symptoms (drowsiness, trouble breathing, seizures), go to urgent care or call emergency services. It’s better to be safe than sorry.
There’s also a new tool: the American Academy of Pediatrics’ Pediatric Medication Safety Calculator app. It asks for the medication name, frequency, and how late you are-and gives you a clear “give” or “skip” answer. Beta testers saw an 83% improvement in decision accuracy. Download it. Save it. Use it.
Why This Matters: Real Consequences
Missed doses don’t just mess up schedules. They cost lives. In the U.S., pediatric medication errors cost $3.5 billion a year. For kids with chronic illnesses like epilepsy, cystic fibrosis, or cancer, missing a dose can mean hospitalization. One parent shared on MedHelp: “My son’s chemo was delayed by 14 hours because I didn’t know the rule. The oncologist said it could reduce his chances of remission.”Parents of children with complex medical needs are 3 times more likely to make medication errors. That’s not because they’re careless. It’s because they’re juggling 4, 5, even 8 different meds a day. Systems fail. Labels confuse. Fatigue sets in. That’s why standardized protocols, visual aids, and clear communication matter more than ever.
The good news? Since 2018, networks of children’s hospitals have cut severe harm from medication errors by 52%. We’re getting better. But it takes every parent knowing the rules.
Final Reminder: When in Doubt, Skip It
You don’t need to be perfect. You just need to be safe. If you’re unsure whether to give the dose or skip it, err on the side of caution. Skip it. Wait for the next scheduled time. Your child’s body will be fine. The next dose will bring them back on track. Doubling up? That’s the real risk.Keep the phone number of your pediatrician’s after-hours line saved. Bookmark the AAP app. Use a syringe. Write it down. And remember: you’re not alone. Thousands of parents face this exact worry every day. You’re doing better than you think.
What should I do if I miss a dose of my child’s antibiotic?
If you miss a dose of an antibiotic, give it as soon as you remember-but only if it’s within half the time until the next dose. For example, if it’s given twice daily (every 12 hours), give it if you’re less than 6 hours late. If it’s been longer, skip it. Never double the dose. Completing the full course is important, but doubling won’t make up for a missed dose and could cause side effects.
Can I give my child the missed dose if it’s almost time for the next one?
No. If it’s within 2 hours of the next scheduled dose (for four-times-daily meds), 3 hours (for three-times-daily), or 6 hours (for twice-daily), skip the missed dose. Giving two doses too close together raises the risk of overdose, especially in children. The body needs time to process the medicine before the next one is given.
Is it safe to use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary in size and can lead to under- or overdosing. The FDA warns that spoon confusion causes 22% of pediatric dosing errors. Always use the oral syringe or dosing cup that came with the medicine. These are calibrated for accuracy.
What if my child’s medication doesn’t have missed-dose instructions on the label?
Many medications-especially high-risk ones-don’t include missed-dose guidance. In fact, 25% of high-risk pediatric drugs lack any instructions on this. Don’t guess. Call your pharmacist or pediatrician. You can also use the AAP’s Pediatric Medication Safety Calculator app for real-time guidance based on the drug and timing.
Should I wake my child up to give a missed dose at night?
Generally, no. If your child is asleep and you realize a dose was missed, don’t wake them unless it’s a critical medication like seizure control or chemotherapy. For most meds, wait until the next scheduled time. Sleep is important for recovery. Waking them up can cause more stress than the missed dose.
How can I reduce the chance of missing doses in the future?
Set phone alarms labeled with the medication name, use a color-coded chart, always measure with an oral syringe, and practice the teach-back method: have someone else show you how to give the dose so you’re sure you understand. For kids on multiple meds, consider a smart dispenser that alerts you when it’s time and tracks what’s been given.



Art Van Gelder
December 23, 2025 AT 05:17Man, I remember when my niece missed her amoxicillin dose and her mom panicked and gave her double. Turned into a vomiting mess at 3 a.m. - ER trip, $800 bill, and now she cries every time she sees a syringe. I swear, the real villain here isn’t the parent - it’s the fact that drug labels assume we’re all pharmacists with PhDs in pediatric dosing. Why isn’t there a universal code? Like, red = skip, green = give? Simple. Visual. No thinking required. We’re overcomplicating survival.
Kathryn Weymouth
December 23, 2025 AT 18:54Thank you for this detailed, accurate breakdown. I’m a pediatric nurse, and I can’t tell you how many parents come in stressed about missed doses - and almost all of them think doubling is the fix. The time-based guidelines you listed are exactly what we teach at Cincinnati Children’s. One thing I’d add: if you’re using a smartphone alarm, set two - one for the dose, one for 15 minutes later as a backup. Sleep is powerful, and so is distraction. You’ll thank yourself later.
Nader Bsyouni
December 25, 2025 AT 02:36Johnnie R. Bailey
December 26, 2025 AT 14:41There’s a quiet dignity in skipping a dose when you’re unsure. No ego. No panic. Just quiet obedience to biology. We treat children like tiny adults because we’re afraid of uncertainty - but their bodies don’t care about our guilt. They only care about rhythm. Give too soon? Overload. Give too late? Underdose. But skip? That’s surrender to nature. And sometimes, that’s the most intelligent thing a parent can do.
Julie Chavassieux
December 26, 2025 AT 15:43Herman Rousseau
December 27, 2025 AT 17:47This is GOLD. 🙌 Seriously, save this post. Print it. Tape it to the fridge next to the syringe. I used the AAP app after my son missed his seizure med - it told me to skip. I did. No drama. No panic. Just calm. Also - color-coded charts? Game changer. We made one with stickers. Now my 4-year-old helps check off doses. He thinks it’s a game. Win-win. 💪
Aliyu Sani
December 28, 2025 AT 09:53Jeremy Hendriks
December 28, 2025 AT 14:15Let’s be real - this whole system is designed to make parents feel guilty. You’re supposed to be perfect. Alarms. Charts. Logs. Syringes. But what about the single mom working two jobs? The dad with PTSD who forgets because he’s hypervigilant? This isn’t medicine - it’s surveillance capitalism dressed in pediatric scrubs. The real solution? Better drug labeling. Not more apps. Not more guilt. Just clarity. And maybe… let people breathe.
Vikrant Sura
December 28, 2025 AT 14:41