Macrolide Therapy Risk Assessment Tool
Patient Risk Assessment
Use this tool to determine if ECG monitoring is recommended for macrolide therapy based on patient characteristics and guidelines.
Risk Assessment Results
Based on your inputs, this patient has a risk score of 0.
QTc Thresholds
Men: >450 ms
Women: >470 ms
These thresholds may trigger discontinuation per UK NHS guidelines
Macrolide antibiotics like azithromycin and clarithromycin treat common infections, but they can dangerously slow your heart’s electrical activity. This is called QT prolongation, which may trigger life-threatening arrhythmias. Here’s who needs ECG monitoring before starting treatment.
What is QT Prolongation and Why Does It Matter?
When your heart’s electrical cycle takes too long to reset between beats, it’s called QT prolongation. This isn’t just a lab curiosity-it can spiral into Torsades de Pointes (TdP), a chaotic heart rhythm that often causes sudden cardiac arrest. A 2012 New England Journal of Medicine study found azithromycin users had a 2.7 times higher risk of cardiovascular death compared to those taking amoxicillin. The macrolide antibiotics include azithromycin, clarithromycin, and erythromycin; they inhibit the hERG potassium channel, disrupting heart rhythm control. Even though the absolute risk of TdP is low (1-8 cases per 10,000 patient-years), it spikes to 3-5% when QTc exceeds 500 ms.
Who Specifically Needs ECG Monitoring?
Not everyone needs an ECG before taking macrolides. Guidelines focus on high-risk groups:
- Women over 65: Female sex increases risk by nearly three times (RR 2.9). Age over 65 doubles it (RR 2.3).
- Those on other QT-prolonging drugs: Taking antidepressants, anti-nausea meds, or antifungals alongside macrolides multiplies danger (RR 4.1).
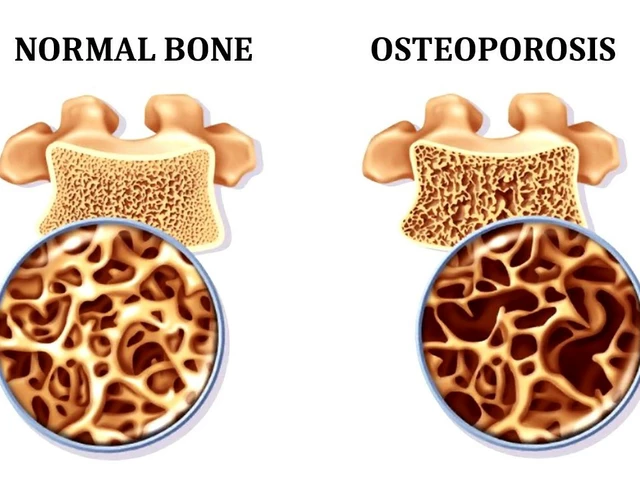
- People with kidney issues: Poor kidney function slows drug clearance, raising blood levels and risk.
- Patients with existing heart conditions: History of arrhythmias or heart failure makes QT prolongation more dangerous.
Consider this real-world example: a 68-year-old woman with baseline QTc of 480 ms developed TdP after five days of clarithromycin, requiring emergency cardioversion. Her case wasn’t unique-Reddit medical forums frequently share similar near-miss stories.
How Guidelines Differ Between Settings
Major guidelines disagree on who should get screened. The British Thoracic Society (BTS) mandates baseline ECG for all patients starting long-term macrolide therapy for respiratory conditions, with QTc thresholds of >450 ms for men and >470 ms for women. Meanwhile, the UK National Health Service says only high-risk patients need checks. This inconsistency shows in practice: specialized respiratory clinics follow BTS guidelines 87% of the time, but primary care settings adhere just 12% of the time.
| Guideline Source | Baseline ECG Requirement | Repeat Monitoring | Key Thresholds |
|---|---|---|---|
| British Thoracic Society (2020) | Required for all long-term therapy | One month after starting | QTc >450 ms (men), >470 ms (women) |
| UK NHS | Only for high-risk patients | As needed based on risk | QTc >500 ms triggers discontinuation |
| NIH (2025) | Risk-stratified approach | Based on risk score changes | 9-point scoring system for personalized decisions |
Why Clinicians Skip ECGs (and What Happens)
Primary care doctors often skip ECGs due to practical hurdles. A 2024 survey of 247 physicians found 65% cited "time constraints," 58% said "lack of clear guidelines for acute infections," and 47% believed "healthy patients face low risk." But skipping checks has consequences. In the UK, routine ECG screening costs £28.50 per test-prohibitively expensive for all 12 million annual macrolide prescriptions. Yet failing to screen misses hidden dangers: BTS data shows 1.2% of screened patients had previously undiagnosed Long QT Syndrome.
Practical Steps for Clinicians
Here’s how to implement monitoring without overwhelming your workflow:
- Check baseline QTc before starting long-term therapy (e.g., for chronic bronchiectasis). Use a corrected QTc value (QTc), not raw QT.
- Use risk scores like the NIH’s 9-point system: assign points for age, sex, kidney function, and other meds.
- Monitor high-risk patients with repeat ECGs at one month. If QTc rises above 500 ms, switch to a safer antibiotic.
- Leverage tech: Epic Systems now auto-alerts doctors when macrolides are prescribed to high-risk patients in 43% of US hospitals.
A 2024 UK hospital study found integrating ECG screening into respiratory clinics added just 8.7 minutes to initial visits but cut adverse events by 34%. That’s a trade-off worth making.
What’s Changing in 2026?
Recent advances are making monitoring easier and smarter. The British Thoracic Society is testing point-of-care QTc devices in 15 clinics-these cut wait times from 5.2 days to under a day. Meanwhile, the American Heart Association’s April 2025 update recommends a risk-stratified approach using a validated 9-point scoring system. This means doctors can skip ECGs for low-risk patients while focusing resources where they matter most. The Institute for Clinical and Economic Review estimates this could save $217 million yearly in the US by preventing arrhythmia complications.
Frequently Asked Questions
Do I need an ECG if I’m healthy and taking azithromycin for a short course?
For short courses (under 5 days) in otherwise healthy patients, guidelines don’t require routine ECGs. But if you have heart conditions, kidney disease, or take other QT-prolonging drugs, discuss testing with your doctor. A 2024 study found 65% of primary care physicians skip ECGs for short courses due to perceived low risk, but exceptions exist for high-risk individuals.
What if my QTc is borderline (470-499 ms)?
Borderline QTc values need careful review. The British Heart Foundation’s online QTc calculator can help interpret results. If your QTc is 470-499 ms, your doctor should check for reversible causes like electrolyte imbalances or drug interactions. Avoid macrolides if possible-switch to alternatives like doxycycline. Studies show 42% of primary care physicians misinterpret borderline values without specialized training.
Can macrolides be safe without an ECG?
Yes, but only for low-risk patients on short courses. The NIH’s 2025 analysis states that "when controlled for underlying comorbidities, macrolide-related arrhythmia risk wasn’t statistically significant" in low-risk groups. However, for patients with multiple risk factors (e.g., women over 65 on multiple QT-prolonging drugs), skipping ECGs is dangerous. Always weigh individual risk factors before deciding.
How do I know if a drug causes QT prolongation?
Check the FDA’s Drug Safety Communications or resources like CredibleMeds.org. For macrolides specifically, azithromycin has a lower risk than erythromycin (OR 1.77 vs 4.82 in meta-analyses). Clarithromycin sits in the middle. Always review all medications a patient takes-combining even low-risk drugs can create dangerous interactions.
Are there alternatives to ECG monitoring?
For high-risk patients, alternatives are limited. Some clinics use continuous cardiac monitors during hospital stays, but outpatient monitoring isn’t feasible yet. The best approach is risk-stratified screening: skip ECGs for low-risk patients but use them for high-risk cases. Emerging point-of-care devices may change this soon-they’re already reducing delays from 5.2 days to 0.8 days in pilot clinics.


Samantha Beye
February 6, 2026 AT 15:43For elderly women on multiple medications, a baseline ECG is essential. I've seen cases where it caught issues early. Always check the risk score before prescribing.
Dr. Sara Harowitz
February 7, 2026 AT 10:33How can doctors even consider skipping ECGs?! It's reckless! The data is clear-QT prolongation kills. Every single high-risk patient needs monitoring. Ignoring this is medical malpractice!
lance black
February 9, 2026 AT 06:42ECG checks save lives. Always do them for high-risk patients.
Carl Crista
February 9, 2026 AT 12:46Big Pharma is hiding the real risks. They want you to think it's safe but the data is skewed. Always check for hidden dangers
Pamela Power
February 11, 2026 AT 04:57'Quick checks' are a joke. Hospitals can't afford it. It's all about money. Real doctors know the risks but the system is broken. You're naive if you think otherwise
one hamzah
February 11, 2026 AT 16:39For Indian patients, kidney issues compound the risk. Always check before prescribing. 🌟 #HealthcareForAll
Diana Phe
February 12, 2026 AT 04:53Big Pharma is behind this. They want to keep us dependent on their drugs. Always check the source! They're lying to us. The real reason for ECGs is to sell more devices. Stay vigilant
Andre Shaw
February 13, 2026 AT 09:28You're dead wrong. It's not about money, it's about patient safety. We need to push for better resources. Stop being so negative! This is life-saving stuff
Laissa Peixoto
February 14, 2026 AT 16:53The cultural context matters.
In some regions, access to ECGs is limited.
We need global solutions.
But maybe it's not just about the test.
It's about understanding the whole picture.
For instance, in India, many patients have kidney issues which compound the risk.
We need to adapt guidelines to local resources.
Also, education for doctors is key.
Many don't know how to interpret QTc properly.
Training programs could help.
It's a systemic issue requiring multiple approaches.
Plus, the cost of ECGs is prohibitive in some areas.
We need to find affordable ways.
Maybe point-of-care devices could help.
But they're not widely available yet.
It's a complex problem.
But the important thing is to not ignore the risks.
Always consider the patient's full picture.
Every detail matters when it comes to heart health.
Rene Krikhaar
February 14, 2026 AT 22:53Always check for drug interactions many patients are on multiple meds a simple ECG can prevent disaster ive seen it happen
anjar maike
February 16, 2026 AT 19:02Short courses are usually safe but always check risk factors. 🌟