COPD Treatment Calculator
Calculate Your COPD Treatment Group
Based on GOLD 2024 guidelines, this calculator helps determine which treatment approach is most appropriate for your COPD.
Use mMRC scale (0-4): 0=No breathlessness, 4=too breathless to leave home
How many moderate-to-severe exacerbations in the past year?
Your COPD Treatment Group
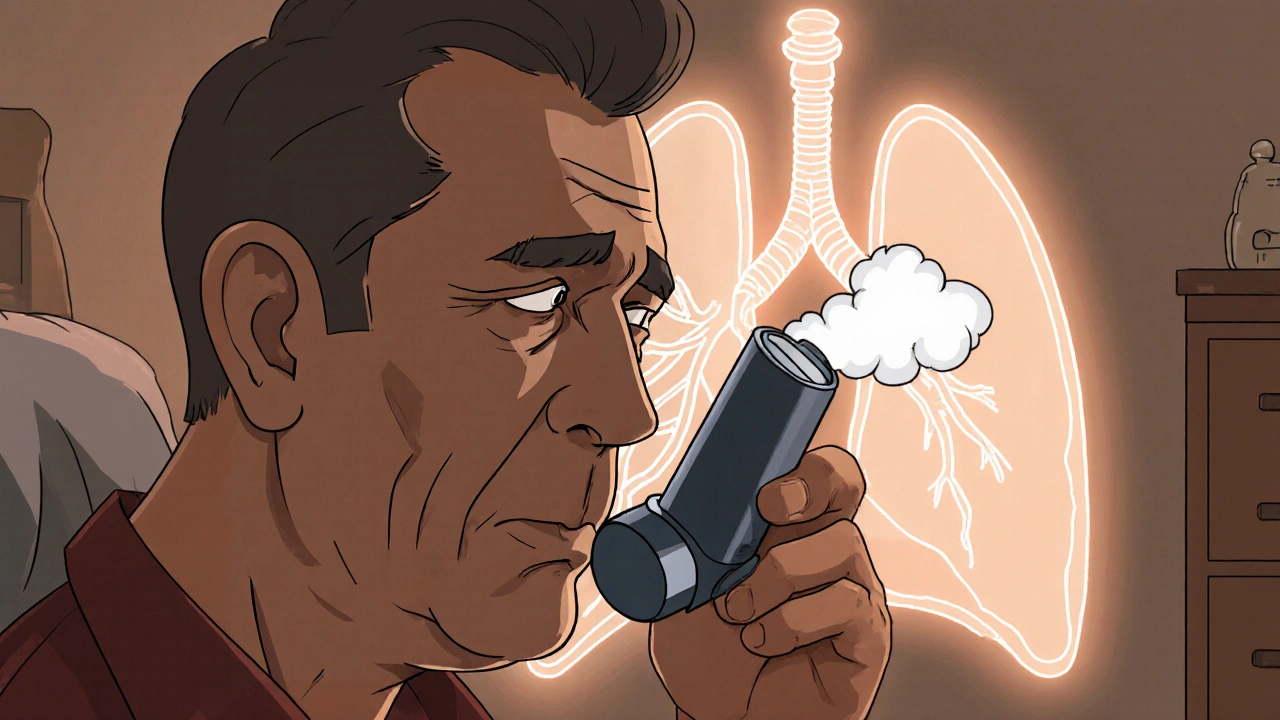
Living with chronic obstructive pulmonary disease (COPD) means dealing with breathlessness, frequent flare‑ups, and a constant battle to keep the lungs clear. One of the most effective weapons in this fight is anticholinergics, a class of drugs that relax airway muscles and improve airflow. This guide breaks down what anticholinergics are, how they fit into modern COPD therapy, and what the latest guidelines say about using them.
Key Takeaways
- Anticholinergics are bronchodilators that block muscarinic receptors, easing airway constriction.
- Long‑acting muscarinic antagonists (LAMAs) such as tiotropium reduce exacerbations and improve quality of life.
- The GOLD 2024 strategy places LAMA therapy as a cornerstone for most symptomatic patients.
- Choosing the right inhaler device and monitoring side effects are crucial for long‑term success.
- Combination therapy with LABA or inhaled corticosteroids may be needed for severe disease.
What Are Anticholinergics?
When you first see the term, it can sound technical, but the concept is simple. Anticholinergics are a group of medications that block the action of acetylcholine at muscarinic receptors in the airways. By doing so, they prevent the muscles surrounding the bronchi from tightening, allowing air to flow more freely. The effect is akin to turning off a faucet that was partially closed, letting the stream of air run unimpeded.
Understanding COPD
Chronic obstructive pulmonary disease is a progressive lung condition characterized by airflow limitation that isn’t fully reversible. Chronic Obstructive Pulmonary Disease encompasses emphysema and chronic bronchitis, leading to chronic cough, sputum production, and shortness of breath. The disease is usually linked to long‑term exposure to irritants like cigarette smoke, and its severity is measured by spirometry, especially the forced expiratory volume in one second (FEV1).
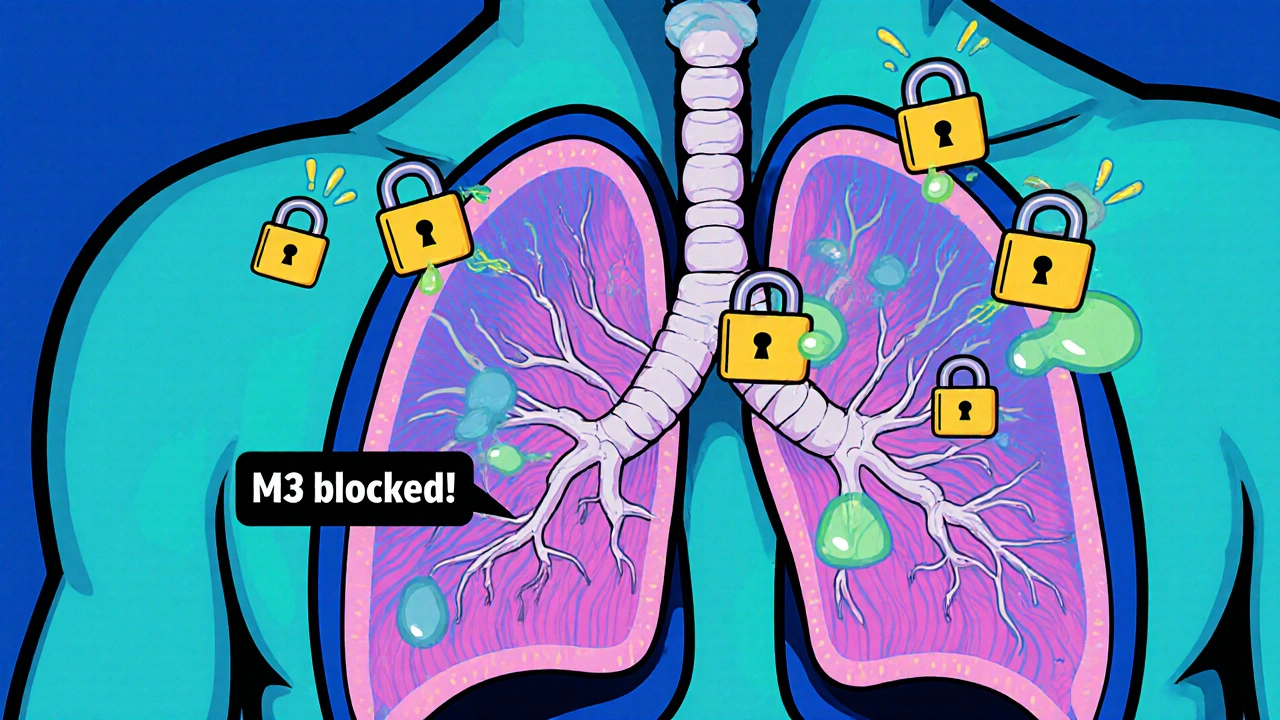
How Anticholinergics Work in the Lungs
Airways contain two main types of muscarinic receptors: M1, which helps regulate mucus secretion, and M3, which drives smooth‑muscle contraction. Anticholinergics preferentially block the M3 receptors, relaxing the bronchial smooth muscle and reducing mucus hypersecretion. This dual action not only opens the airways but also eases cough by limiting excess mucus.
Types of Anticholinergic Bronchodilators
Modern COPD therapy distinguishes between short‑acting and long‑acting agents.
- Short‑acting muscarinic antagonists (SAMA): Typically used for quick relief, examples include ipratropium bromide.
- Long‑acting muscarinic antagonists (LAMA): Designed for maintenance therapy, they provide bronchodilation for 24 hours or more. Key LAMAs are:
- Tiotropium (HandiHaler or Respimat)
- Umeclidinium (Anoro™ Ellipta)
- Aclidinium (Tudorza Pressair™)
- Glycopyrronium (Seebri™ Breezhaler)
Among these, tiotropium remains the most studied, with robust data showing reductions in exacerbations, hospitalizations, and mortality.
Clinical Evidence & Guidelines
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines are the gold standard for COPD management. The 2024 GOLD report categorizes patients into four groups (A‑D) based on symptom burden (using the mMRC or CAT scores) and exacerbation risk. For groups B, C, and D-those with higher symptoms or exacerbation risk-GOLD recommends a LAMA as first‑line maintenance therapy.
Key trials that shaped these recommendations include:
- The UPLIFT study (2008) which followed 5,993 patients on tiotropium for four years, showing a statistically significant 12% reduction in moderate-to-severe exacerbations.
- The SHINE trial (2015) comparing tiotropium with salmeterol (a LABA) demonstrated superior lung‑function improvement with the LAMA.
- The QUANTIFY‑COPD meta‑analysis (2023) pooled data from 12 LAMA trials, confirming an average increase of 0.11 L in FEV1 and a 15% lower risk of hospitalization.
These findings cement LAMAs as a cornerstone of COPD treatment, especially for patients who experience frequent flare‑ups.
Comparing Anticholinergics with Other COPD Therapies
| Class | Typical Onset | Duration of Action | Common Dosing Frequency | Main Benefit | Typical Side Effects |
|---|---|---|---|---|---|
| LAMA (e.g., tiotropium) | 15‑30 min | 24 h+ | Once daily | Reduced exacerbations, improved FEV1 | Dry mouth, urinary retention |
| SAMA (e.g., ipratropium) | 5‑10 min | 4‑6 h | Every 4-6 h | Quick relief of bronchoconstriction | Cough, throat irritation |
| LABA (e.g., salmeterol) | 10‑15 min | 12 h | Twice daily | Rapid bronchodilation, symptom control | Tremor, palpitations |
| ICS (e.g., fluticasone) | 30‑60 min | 24 h | Once or twice daily | Decreases airway inflammation | Oropharyngeal candidiasis, hoarseness |
| LAMA + LABA combo (e.g., umeclidinium + vilanterol) | 15‑20 min | 24 h | Once daily | Synergistic bronchodilation, greater FEV1 gain | Combined side‑effect profile |
When you weigh the options, anticholinergic LAMAs stand out for their once‑daily dosing and strong evidence for preventing exacerbations, making adherence easier for many patients.
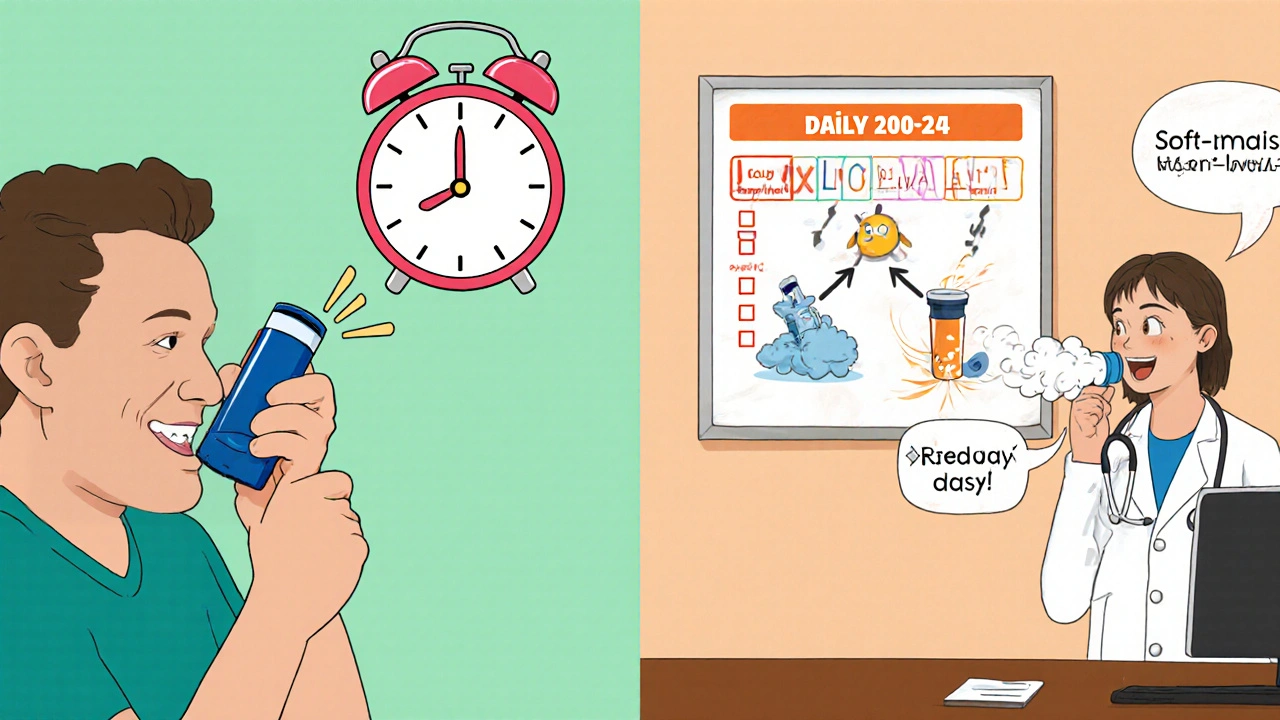
Practical Tips for Using Anticholinergics
- Choose the right inhaler device. Dry‑powder inhalers (DPIs) like the Ellipta require a forceful breath, whereas soft‑mist inhalers (Respimat) generate a fine aerosol that can be easier for older adults.
- Master inhalation technique. Exhale fully, seal lips around the mouthpiece, inhale deeply and hold breath for about 10 seconds before exhaling slowly.
- Set a daily reminder. Because LAMAs are taken once a day, tying the dose to a routine activity (e.g., brushing teeth) reduces missed doses.
- Track symptom changes. Use a simple diary or a mobile app to note CAT scores, rescue inhaler use, and any side effects.
- Schedule regular spirometry. Objective lung‑function tests every 6‑12 months help gauge treatment response and guide escalation.
Potential Side Effects & Safety Concerns
While anticholinergics are generally well tolerated, clinicians keep an eye on a few common issues:
- Dry mouth (xerostomia). Often mild; sipping water or using sugar‑free gum can help.
- Urinary retention. More relevant for men with enlarged prostate; discuss alternative agents if problematic.
- Constipation. Increase dietary fiber and fluids.
- Cardiovascular risk. Large trials have not shown a significant increase, but patients with uncontrolled arrhythmias should be monitored.
If any side effect becomes severe or interferes with daily life, contact a healthcare professional promptly; dose adjustment or switching to another inhaler may resolve the issue.
Frequently Asked Questions
Can I use a SAMA and a LAMA together?
Generally no. Both drugs block muscarinic receptors, so using them together offers little additional benefit and raises the risk of side effects like dry mouth. If a patient needs extra relief, a LABA or combination inhaler is usually preferred.
How quickly will I feel better after starting a LAMA?
Most patients notice symptom improvement within a week, with peak lung‑function gains around 2‑4 weeks. Full benefit in reducing exacerbations may take several months, which is why doctors monitor outcomes over time.
Are anticholinergics safe for people with heart disease?
Large studies, including the UPLIFT trial, have not found a meaningful increase in cardiovascular events among COPD patients on LAMAs. Still, doctors evaluate each case individually, especially if the patient has recent heart failure or uncontrolled arrhythmias.
Do anticholinergics work for asthma?
They are not first‑line for asthma because airway inflammation is the primary driver. However, a SAMA like ipratropium can be added during severe exacerbations under medical supervision.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and continue with your regular schedule. Never double‑dose.


John Price
October 21, 2025 AT 17:57LAMS are great for once‑daily dosing, keep the lungs open.
Vivian Annastasia
October 22, 2025 AT 10:37Oh, look at you, discovering that inhalers work.
Sure, because breathing is such a novel concept for most of us, right?
Ericka Suarez
October 23, 2025 AT 03:17Wow, this is a total game changer!
I cant beleive how simple it is to just press a button and BREATHE.
Honestly these meds are a miracle for america and its great people.
Everyone should jump on the bandwagon now, no excuses!
Esther Olabisi
October 23, 2025 AT 19:57Haha, totally agree, it’s like a magic wand for lungs 😏.
Keep pushing those inhalers, folks, you’ll be fine! 😊
Jake Hayes
October 24, 2025 AT 12:37That’s a simplistic view. The evidence clearly supports LAMA superiority over SAMA.
parbat parbatzapada
October 25, 2025 AT 05:17They dont want us to know the real truth. All these pharma giants push LAMAs to keep us hooked on their profit machine.
Think about the data they hide, the side effects they sweep under the rug.
It’s all a grand control scheme, don’t you see?
Casey Cloud
October 25, 2025 AT 21:57The guidelines are based on large randomized trials that showed consistent reductions in exacerbations.
Tiotropium has the most robust safety profile when used as directed.
Patients should follow the inhaler technique instructions for best results.
Rachel Valderrama
October 26, 2025 AT 13:37Wow, so now we’re all health gurus!
Just remember to breathe in, breathe out, and keep that optimism cranked up!
Brandy Eichberger
October 27, 2025 AT 06:17One must appreciate the nuanced pharmacodynamics of anticholinergic agents.
It’s truly a marvel of modern medicine, wouldn’t you agree?
Chirag Muthoo
October 27, 2025 AT 22:57I concur wholeheartedly that the scientific community has made commendable progress in COPD management.
Let us continue to encourage patients to adhere to evidence‑based therapies.
Ashok Kumar
October 28, 2025 AT 15:37It’s nice you’re so optimistic, but let’s not pretend the side‑effects are trivial.
Dry mouth can be a real nuisance for many.
Ivan Laney
October 29, 2025 AT 08:17Allow me to set the record straight regarding the monumental impact of anticholinergic bronchodilators on chronic obstructive pulmonary disease management. The United States, a beacon of medical innovation, has led the charge in adopting long‑acting muscarinic antagonists as first‑line therapy for symptomatic patients. This strategic decision stems from the robust body of evidence gathered over decades, beginning with the landmark UPLIFT trial that demonstrated a 12 % reduction in moderate‑to‑severe exacerbations among thousands of participants. Subsequent investigations, such as the SHINE and QUANTIFY‑COPD studies, reinforced the superiority of LAMAs in improving forced expiratory volume and curbing hospital admissions. Moreover, real‑world data have consistently shown that once‑daily dosing enhances adherence, a critical factor when dealing with a disease that often plagues the elderly. The pharmacodynamic profile of agents like tiotropium, ulecidinium, and glycopyrronium ensures prolonged bronchodilation by selectively antagonizing M3 receptors while sparing M2‑mediated feedback mechanisms. This specificity translates to a favorable safety canvas, with adverse events limited primarily to dry mouth and occasional urinary retention, both manageable with simple interventions. Moreover, the integration of LAMAs with long‑acting beta‑agonists or inhaled corticosteroids creates a synergistic effect, delivering unparalleled lung‑function gains and quality‑of‑life improvements. It is incumbent upon clinicians, especially those practicing in the great American heartland, to personalize inhaler device selection-recognizing that dry‑powder inhalers demand a robust inspiratory flow, whereas soft‑mist devices may suit patients with reduced inspiratory capacity. Education on proper technique, coupled with reminders anchored to daily routines, can dramatically reduce missed doses. Regular spirometric monitoring every six to twelve months further optimizes therapeutic pathways, allowing for escalation when necessary. Let us not forget that while anticholinergics are pivotal, they are but a component of a comprehensive management plan that includes smoking cessation, pulmonary rehabilitation, and vaccination strategies. In sum, the unparalleled efficacy, safety, and convenience of anticholinergic LAMAs solidify their status as the cornerstone of contemporary COPD therapy-an achievement that reflects the ingenuity and dedication of American medical research and practice.