Metoclopramide-Antipsychotic Interaction Risk Calculator
Important: This tool assesses risk based on medication combinations and factors discussed in the article. It does not replace professional medical advice. Always consult your healthcare provider before changing medications.
Your Medications
Risk Assessment
Important Information
Neuroleptic Malignant Syndrome (NMS) is a medical emergency. If you experience fever, muscle stiffness, confusion, rapid heart rate, or dark urine, seek immediate medical attention.
The FDA strongly recommends avoiding metoclopramide in patients taking antipsychotics or other dopamine-blocking medications due to the high risk of NMS.
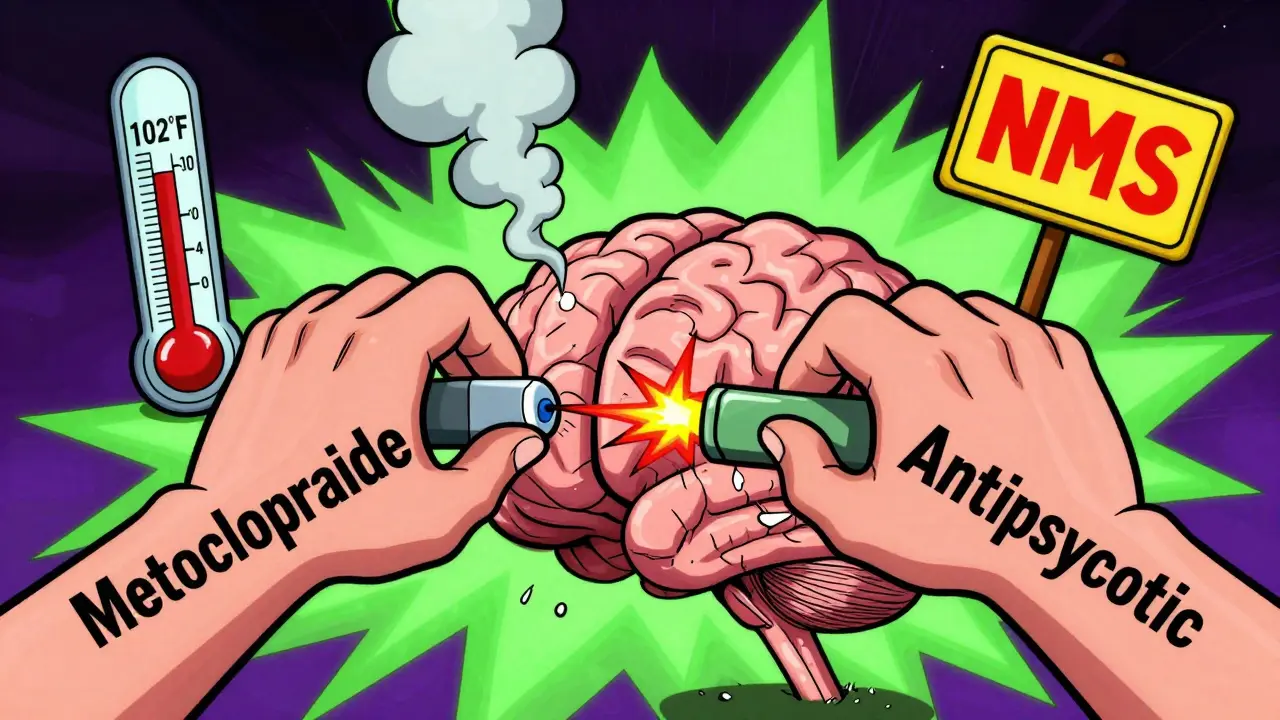
Combining metoclopramide with antipsychotic medications isn’t just a minor caution-it’s a potentially deadly mix. If you or someone you know is taking both, you need to understand what’s really going on inside the body. This isn’t about side effects you might read about on a pill bottle. This is about Neuroleptic Malignant Syndrome, a rare but life-threatening condition that can strike without warning.
What Metoclopramide Does to Your Brain
Metoclopramide, sold under brand names like Reglan and Gimoti, is a drug meant to help with nausea and slow stomach emptying. It works by blocking dopamine receptors in the brain’s vomiting center and speeding up digestion. Sounds simple enough. But dopamine isn’t just about nausea. It’s a key player in movement, mood, and how your brain communicates with your muscles. The problem? Metoclopramide doesn’t just block dopamine in the gut. It crosses into the brain and blocks dopamine receptors there too. That’s why it can cause tremors, muscle stiffness, and even involuntary movements. The FDA has put a Boxed Warning on metoclopramide because of this. Long-term use, especially beyond 12 weeks, can lead to tardive dyskinesia-a movement disorder that may never go away.How Antipsychotics Work-And Why That’s a Problem
Antipsychotics like haloperidol, risperidone, and olanzapine were designed to treat schizophrenia and bipolar disorder. They work by blocking dopamine receptors in the brain to reduce hallucinations and delusions. That’s their job. But that same mechanism is what makes them dangerous when mixed with metoclopramide. Think of it like two people trying to turn off the same light switch at the same time. Both drugs are blocking dopamine receptors. Together, they don’t just double the effect-they can overload the system. The brain’s dopamine pathways get so suppressed that muscles lock up, body temperature spikes, and the nervous system starts to shut down. That’s Neuroleptic Malignant Syndrome.What Is Neuroleptic Malignant Syndrome (NMS)?
NMS isn’t just a bad reaction. It’s a medical emergency. It happens when dopamine activity in the brain drops too low, too fast. The classic signs are a four-part warning: high fever (often above 102°F), rigid muscles, confused or changing mental status, and unstable blood pressure or heart rate. You might also see rapid breathing, sweating, and dark urine from muscle breakdown. The scary part? NMS can develop within days of starting or increasing the dose of either drug. It’s rare-only about 0.02% to 0.05% of people on antipsychotics get it-but the death rate is 10% to 20% if not treated immediately. And when metoclopramide is added, the risk isn’t just higher-it’s predictable. The FDA’s prescribing information for Reglan is blunt: Avoid Reglan in patients receiving other drugs associated with NMS, including typical and atypical antipsychotics. That’s not a suggestion. That’s a red flag.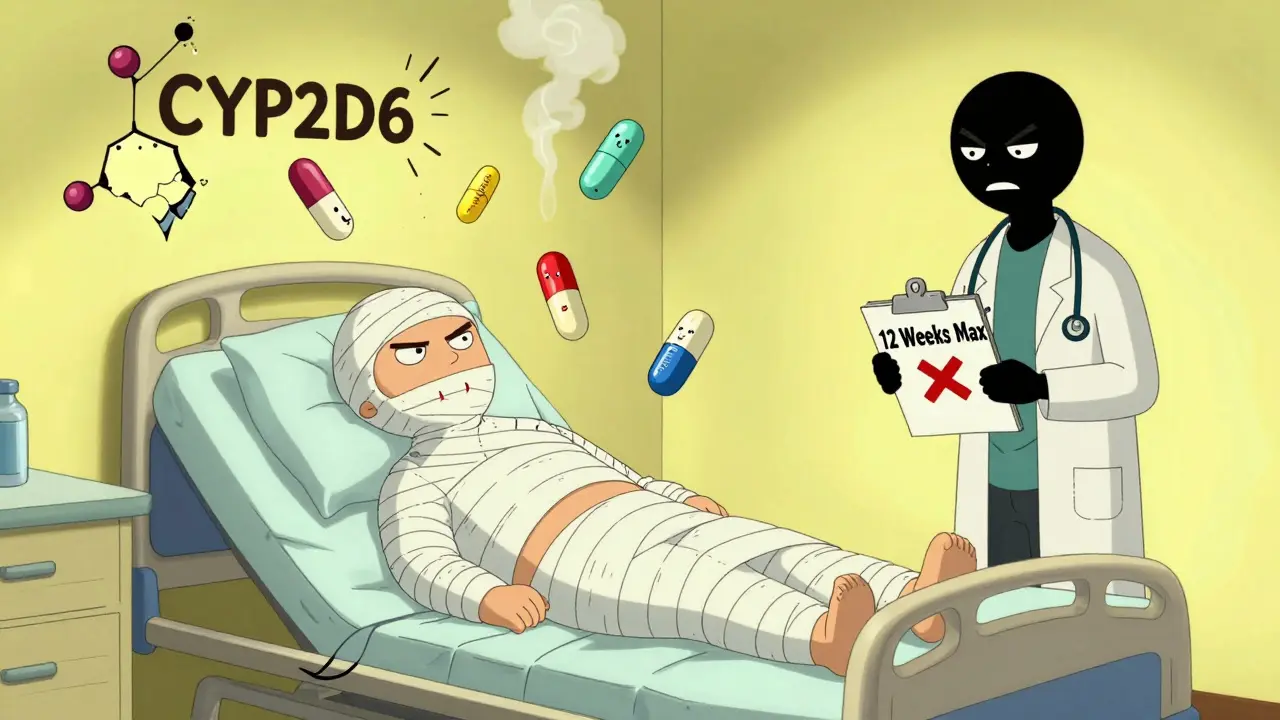
Why This Interaction Is Worse Than You Think
It’s not just about both drugs blocking dopamine. There’s another layer. Many antipsychotics, especially older ones like haloperidol and newer ones like risperidone, block the CYP2D6 enzyme in the liver. That’s the same enzyme that breaks down metoclopramide. So now you’ve got a double hit:- Pharmacodynamic hit: Both drugs are blocking dopamine receptors in the brain.
- Pharmacokinetic hit: The antipsychotic slows down how fast your body clears metoclopramide, so more of it builds up in your system.
Who’s Most at Risk?
Some people are far more likely to develop NMS from this combo:- Older adults-metabolism slows down, and dopamine pathways are already more fragile.
- People with kidney problems-metoclopramide is cleared by the kidneys. If they’re not working well, the drug builds up.
- People with genetic CYP2D6 deficiency-about 7% of Caucasians and 2% of Asians have this. Their bodies can’t break down metoclopramide at all.
- Those with a history of movement disorders-like Parkinson’s disease or prior tardive dyskinesia.
- Patients on high doses of antipsychotics or recently started on them.
What Should You Do Instead?
If you’re on an antipsychotic and need help with nausea or gastroparesis, metoclopramide is not the answer. There are safer alternatives:- Ondansetron (Zofran)-blocks serotonin, not dopamine. Safe with antipsychotics.
- Meperidine-for severe nausea, though not for long-term use.
- Prochlorperazine-yes, it’s also a dopamine blocker, but it’s used differently and with more caution. Still, ondansetron is preferred.
- Non-drug options-acupuncture, ginger, small frequent meals, avoiding triggers.
What If You’re Already Taking Both?
If you’re currently on metoclopramide and an antipsychotic, don’t stop suddenly. That can cause withdrawal symptoms or rebound nausea. Talk to your doctor or pharmacist right away. Ask these questions:- Is there a safer alternative for my nausea or stomach issue?
- How long have I been on metoclopramide? Am I past the 12-week safety limit?
- Do I have any signs of movement problems-tremors, stiffness, or odd facial movements?
- Am I taking any other meds that block CYP2D6, like fluoxetine or bupropion?
The Bottom Line
This isn’t a theoretical risk. It’s a documented, preventable tragedy. The FDA, academic journals, and clinical guidelines all agree: don’t mix metoclopramide with antipsychotics. The combination can kill. If you’re a patient, speak up. Bring a list of all your medications to every appointment. If you’re a caregiver, watch for sudden stiffness, fever, or confusion. If you’re a healthcare provider, don’t assume someone’s “just getting a little nausea relief.” That little pill can be the trigger for a full-blown crisis. Metoclopramide has its place-for short-term use in people who aren’t on antipsychotics. But when dopamine-blocking drugs stack up, the brain can’t cope. The body pays the price.Frequently Asked Questions
Can metoclopramide cause Neuroleptic Malignant Syndrome on its own?
Yes, but it’s rare. Metoclopramide alone can trigger NMS, especially at high doses or in people with kidney problems or genetic enzyme deficiencies. However, the risk increases dramatically when combined with antipsychotics or other dopamine-blocking drugs. The FDA warns against using it with any drug linked to NMS, including antipsychotics, because the combination is far more dangerous.
How quickly can NMS develop after taking both drugs?
NMS can develop within hours to days after starting or increasing the dose of either drug. In some cases, symptoms appear within 24 to 72 hours. There’s no safe waiting period-this isn’t a risk that builds slowly over months. If you’re on both drugs and suddenly feel stiff, feverish, or confused, seek emergency help immediately.
Is there a blood test to detect NMS risk before it happens?
No blood test can predict NMS before it starts. But doctors can check creatine kinase (CK) levels if symptoms appear-high CK signals muscle breakdown, a key sign of NMS. Genetic testing for CYP2D6 enzyme activity is available but not routine. The best prevention is avoiding the drug combo altogether, especially in high-risk patients.
What should I do if I’ve been on metoclopramide for more than 12 weeks?
Stop taking it and talk to your doctor. The FDA’s Boxed Warning says metoclopramide should not be used for longer than 12 weeks because of the risk of tardive dyskinesia-a permanent movement disorder. If you’re also on an antipsychotic, the risk of NMS rises sharply. Your doctor can help you switch to a safer alternative like ondansetron or adjust your treatment plan.
Can I take metoclopramide if I’ve had tardive dyskinesia before?
No. If you’ve ever had tardive dyskinesia from any drug-including metoclopramide, antipsychotics, or other dopamine blockers-you should never take metoclopramide again. WebMD and the FDA both list this as a strict contraindication. Tardive dyskinesia can worsen or become permanent, and the risk of NMS is too high to justify any further exposure.



anthony epps
December 17, 2025 AT 07:11So if you’re on antipsychotics and get sick, just grab Zofran instead? That sounds way safer.
Kim Hines
December 18, 2025 AT 06:33I’ve seen this happen to a friend. They didn’t know the combo was dangerous until they ended up in ICU. Never again.
Ron Williams
December 19, 2025 AT 07:28This is exactly why we need better communication between specialists. GI docs prescribe Reglan. Psych docs prescribe antipsychotics. Nobody talks. And the patient pays the price.
Josias Ariel Mahlangu
December 19, 2025 AT 11:46People treat medication like candy. This isn’t a suggestion-it’s a death sentence waiting to happen. If you don’t read the warnings, you deserve what you get.
sue spark
December 19, 2025 AT 18:59I’m so glad someone finally put this out there. So many people are suffering silently because no one told them this could happen. Knowledge is power
Tiffany Machelski
December 20, 2025 AT 15:51My mom was on this combo for months. She started twitching and couldn’t walk. We didn’t connect it until the ER doctor asked about her meds. Never again.
James Rayner
December 22, 2025 AT 14:58It’s terrifying how easily a well-intentioned treatment can become a trap. Dopamine isn’t just a chemical-it’s the thread holding movement, thought, and feeling together. Pull it too tight, and the whole system unravels.
And yet, we keep prescribing like we’re playing chess with lives. One move here, one move there-no one sees the checkmate coming.
Maybe the real problem isn’t the drugs. It’s the system that lets them cross paths without warning.
I’ve sat with patients who woke up paralyzed after a simple nausea pill. No scream. No warning. Just silence.
And then the guilt. The family asking, ‘Why didn’t anyone tell us?’
We need better alerts. Better training. Better empathy.
Not just in the script-but in the soul of medicine.
This post? It’s not just information. It’s a lifeline.
Thank you.
Souhardya Paul
December 22, 2025 AT 21:34Just had a patient come in last week with elevated CK and rigidity after starting Reglan for gastroparesis. He was on risperidone. We pulled both meds immediately. He’s recovering, but barely. This is real.
Also, domperidone is available through special access programs in the US-ask your pharmacist. It’s not impossible to get.
Hadi Santoso
December 22, 2025 AT 23:43wait so prozac + antipsychotic + reglan = triple threat?? i had no idea… my aunt takes all three and gets really tired all the time… maybe its not just aging??
Aditya Kumar
December 23, 2025 AT 02:59Too much info. Just tell me what to avoid.
SHAMSHEER SHAIKH
December 23, 2025 AT 22:05This is not merely a pharmacological interaction-it is a systemic failure of medical education, regulatory oversight, and clinical vigilance. The FDA’s boxed warning exists, yet prescribers continue to overlook it as if it were a footnote in a textbook. The confluence of pharmacodynamic and pharmacokinetic synergism, particularly in CYP2D6-deficient populations, is not speculative-it is empirically documented in peer-reviewed literature spanning decades. Yet, in primary care settings, metoclopramide is still dispensed like an over-the-counter antacid. This is not negligence; it is institutionalized complacency. The cost? Human lives. The solution? Mandatory CPOE alerts, mandatory continuing education on polypharmacy risks, and a cultural shift away from prescribing convenience toward pharmacological humility. We must stop treating patients as data points and start treating them as complex biological systems. One pill may seem harmless. Two may seem routine. Three? That is where the abyss begins.
Cassandra Collins
December 25, 2025 AT 06:11you know what’s really scary? i think big pharma knows this and doesn’t care. they make billions off antipsychotics and reglan. if everyone knew this combo could kill, they’d stop using it. but then who’d buy the next drug? they’d rather keep people sick and dependent. i’m not crazy. check the lawsuits. they’ve been hiding this for years.