When you hear Ranitidine is a histamine‑2 (H2) receptor antagonist that was widely used to lower stomach acid and treat heartburn, ulcers, and gastro‑esophageal reflux disease (GERD), you probably remember it as the over‑the‑counter Zantac you could pick up at the pharmacy. That familiarity vanished quickly after 2020 when the FDA announced a massive recall because of a probable carcinogen called NDMA (N‑nitrosodimethylamine). Since then, patients and doctors have been hunting for safe, effective backups. This guide walks you through the most common alternatives, compares how they stack up on key factors, and helps you decide which option fits your needs without the lingering worries about ranitidine’s safety.
How Ranitidine Works (and Why It Fell Out of Favor)
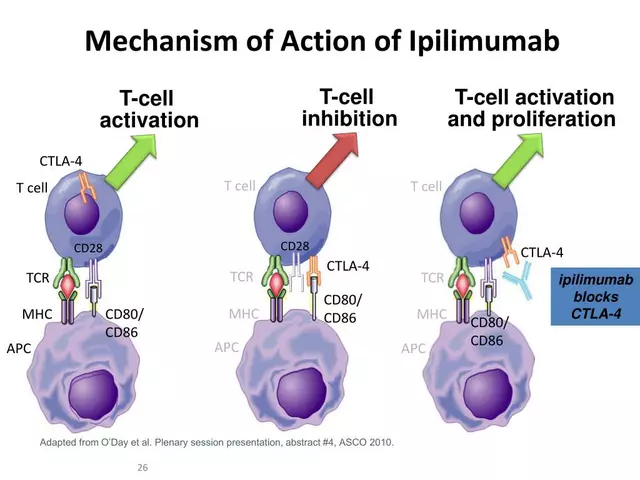
Ranitidine blocks the H2 receptors on stomach lining cells, preventing histamine from triggering acid production. The result is a modest reduction in gastric acid, enough to give relief from mild‑to‑moderate heartburn within 30‑60 minutes. Because it works at the receptor level, its effects wear off after about 8‑12hours, meaning most users take it twice daily.
Two things led to its downfall. First, routine testing revealed that even at standard storage temperatures, ranitidine could break down into NDMA, a substance linked to liver and kidney cancers. Second, the FDA’s risk assessment suggested that long‑term exposure, even at low levels, might exceed acceptable limits. The agency’s 2020 recall forced manufacturers to pull the product worldwide, leaving a gap for patients who still need acid‑suppressing therapy.
Top Alternatives to Ranitidine
When you’re looking for a substitute, think of three main families:
- Famotidine - another H2 blocker with a better safety record and less NDMA formation.
- Cimetidine - the older H2 antagonist; effective but interacts with several drugs.
- Proton‑pump inhibitors (PPIs) like omeprazole - they act deeper in the acid‑production pathway, offering stronger and longer relief.
There’s also nizatidine, a lesser‑known H2 blocker available in some markets, and newer “dual‑action” combos that pair an H2 blocker with an antacid. The choice depends on how severe your symptoms are, whether you’re on other meds, and your tolerance for potential side effects.
Detailed Comparison Table
| Drug | Drug Class | Typical Dose (Adults) | Onset of Relief | Duration of Action | Major Safety Concerns | Average Cost (NZD per month) |
|---|---|---|---|---|---|---|
| Ranitidine | H2 blocker | 150mg twice daily | 30‑60min | 8‑12h | NDMA impurity risk; withdrawn from market | ~$10 |
| Famotidine | H2 blocker | 20‑40mg once daily | 30‑45min | 10‑12h | Generally safe; rare headache, dizziness | ~$12 |
| Cimetidine | H2 blocker | 200‑400mg twice daily | 30‑60min | 6‑8h | Drug‑drug interactions (e.g., warfarin, theophylline) | ~$8 |
| Omeprazole | Proton‑pump inhibitor | 20mg once daily | 1‑2h | 24h+ | Long‑term risk of bone fractures, B12 deficiency | ~$15 |
When to Choose an H2 Blocker vs. a Proton‑Pump Inhibitor
If your symptoms flare up occasionally-think weekend binge drinking or a spicy dinner-an H2 blocker like famotidine usually does the trick. They act fast, are cheap, and have fewer long‑term concerns. However, they only cut acid production by about 30‑40%.
For chronic GERD, erosive esophagitis, or ulcer healing, a PPI offers up to 90% suppression. The trade‑off is a slower onset and the need to stay on the drug for weeks or months. Recent guidelines suggest using the lowest effective PPI dose and stepping down to an H2 blocker for maintenance when possible.
One practical rule of thumb: if you need relief within an hour and plan to use the medication for less than two weeks, start with an H2 blocker. If symptoms persist beyond that, talk to your doctor about switching to a PPI.
Safety Tips & Monitoring for Each Option
Regardless of which drug you pick, keep these checkpoints in mind:
- Check for interactions. Cimetidine is a known CYP450 inhibitor; it can raise levels of anticoagulants, anti‑seizure meds, and certain antidepressants.
- Watch for side‑effects. Famotidine can cause mild headache or dizziness. PPIs may lead to occasional constipation or diarrhea.
- Regular labs. If you’re on a PPI longer than six months, ask your doctor to test B12 and magnesium levels.
- Age considerations. Older adults are more prone to PPI‑related bone density loss; an H2 blocker might be safer.
- Pregnancy & lactation. Famotidine is classified as pregnancy‑category B and is generally preferred over cimetidine (category C) and PPIs (category C‑D).
For anyone who previously took ranitidine, there’s no need for a “detox” period-just switch to the new drug and monitor symptom control. If you experience new or worsening pain, contact a healthcare professional promptly.

Choosing the Right Alternative for You
Let’s break down decision factors with a quick checklist you can run through during your next pharmacy visit:
- Symptom frequency: Occasional → H2 blocker; Daily → consider PPI.
- Current medications: If you’re on warfarin, try famotidine over cimetidine.
- Cost sensitivity: Cimetidine is usually cheapest, but the price gap with famotidine is small in NZ.
- Long‑term health goals: Avoid PPIs if you have osteoporosis risk.
- Allergy history: Rarely, patients react to the sulfonyl group in some H2 blockers; an alternative class is safest.
Use this matrix as a mental guide, then discuss it with your pharmacist or doctor. Most insurers in NewZealand cover famotidine and PPIs, so cost rarely becomes a blocker.
Real‑World Stories: How People Switched After the Recall
Emma, a 42‑year‑old teacher from Wellington, relied on ranitidine for seasonal acid reflux. After the 2020 recall, she tried an over‑the‑counter famotidine tablet. Within three days, her heartburn frequency dropped from five episodes a day to one. She appreciated the once‑daily dosing and reported no headaches.
Mark, a 67‑year‑old retiree on multiple anticoagulants, couldn’t risk cimetidine’s interaction profile. His doctor prescribed omeprazole for eight weeks, then tapered him to famotidine for maintenance. Six months later, his endoscopy showed healed esophageal lining, and his bone‑density scan remained stable.
These anecdotes illustrate that the “best” alternative really depends on individual health context-not just price or brand fame.
Frequently Asked Questions
Is famotidine a safe replacement for ranitidine?
Yes. Famotidine is an H2 blocker that does not form NDMA under normal storage conditions, making it a widely accepted alternative after the ranitidine recall.
Can I take an H2 blocker and a PPI at the same time?
Usually there’s no benefit in combining them because they work on the same pathway. In rare cases, a doctor might prescribe both for severe ulcer disease, but this should be closely monitored.
What should I do if I experience persistent heartburn after switching?
First, verify you’re taking the correct dose and timing. If symptoms continue for more than two weeks, schedule a visit to rule out underlying conditions like a hiatal hernia or ulcer.
Are there any natural alternatives to ranitidine?
Lifestyle tweaks-elevating the head of the bed, eating smaller meals, avoiding caffeine and alcohol-can reduce acid reflux. Herbal teas with ginger or licorice (DGL) may provide mild relief, but they’re not a substitute for prescription‑grade acid suppression when you have severe disease.
How long is it safe to stay on a PPI?
Guidelines suggest limiting continuous PPI use to 8‑12 weeks unless a doctor monitors you for complications. If long‑term therapy is needed, periodic assessment of bone density, magnesium, and B12 levels is recommended.


Edward Morrow
October 12, 2025 AT 04:34Man, the whole ranitidine fiasco was a perfect example of how the U.S. pharma watchdogs actually give a damn about consumer safety while the rest of the world just chases cheap knock‑offs. The FDA’s swift recall saved a ton of lives, and anyone still whining about “availability” is just clueless or buying into foreign junk. If you’re still hunting for a cheap over‑the‑counter fix, pick famotidine – it’s the real American‑made hero that doesn’t turn your stomach into a chemical crime scene. Trust the home‑grown science, not that sketchy imported stuff.
Shayne Tremblay
October 12, 2025 AT 15:40Switching away from ranitidine can feel a bit daunting, but think of it as a chance to upgrade your gut health routine! Famotidine and the newer PPIs have solid safety records, and many users report smoother evenings with fewer heartburn spikes. Keep an eye on dosages, stay hydrated, and don’t hesitate to chat with your pharmacist – they’ll help you pick the right fit for your lifestyle. You’ve got this, and your stomach will thank you for the fresh start.
Stephen Richter
October 13, 2025 AT 02:47It is advisable, when substituting ranitidine, to consider pharmacokinetic profiles in order to optimise therapeutic outcomes. Famotidine demonstrates a longer half‑life and reduced risk of nitrosamine formation. Moreover, cimetidine’s cytochrome P450 inhibition warrants caution in polypharmacy scenarios. Patients encountering persistent dyspepsia should undergo endoscopic evaluation according to established guidelines.
Musa Bwanali
October 13, 2025 AT 13:54Spot on, Stephen! I’d add that for folks who only get the occasional burn, the quick kick‑in of famotidine can be a real game‑changer, saving them from a night of tossing and turning. Just remember not to overdo it – the goal is relief, not dependence. Keep the dosage low, and if you’re still battling symptoms after a week, it might be time to talk to a doc about stepping up to a PPI.
Allison Sprague
October 14, 2025 AT 01:00Let’s be crystal clear: the hype around “natural” antacids is often just marketing fluff, and anyone still clutching at herbal teas as a cure‑all is ignoring hard data. Clinical trials consistently show that H2 blockers like famotidine outperform over‑the‑counter antacids in both onset speed and duration. If you’re counting pennies, cimetidine is cheap, but its interaction profile is a minefield – you don’t want your blood thinner spiking because of a cheap heartburn pill. Bottom line: stick to evidence‑based meds, monitor side effects, and don’t let anecdotal “miracle cures” steer your health decisions.
leo calzoni
October 14, 2025 AT 12:07Honestly, the science is obvious. Famotidine is superior; it does not produce NDMA and works faster. Anything else is just a downgrade.
KaCee Weber
October 14, 2025 AT 23:14While I respect the straightforward confidence in famotidine’s profile, it’s worth remembering that medication choices often intersect with personal, cultural, and economic factors, and a one‑size‑fits‑all declaration can unintentionally marginalize those whose circumstances differ from the ideal scenario presented 👐. For instance, a patient in a remote community might have limited access to famotidine and therefore rely on cimetidine despite its interaction risks, simply because it’s the only H2 blocker stocked at the local clinic 🏥. Moreover, the cost‑benefit analysis isn’t purely about drug price; it also encompasses the cost of additional lab monitoring, potential hospital visits due to side‑effects, and the intangible burden of anxiety when choosing a medication that feels “risky” 🤔. In this vein, some individuals find comfort in the long‑standing presence of cimetidine in their treatment history, especially if they’ve built a therapeutic rapport with their physician around that regimen. It’s also important to note that the pharmacogenomic landscape is evolving, and future studies may identify subpopulations who metabolize certain H2 blockers more efficiently, which could shift current preferences dramatically 🌐. From a holistic perspective, encouraging patients to discuss their lifestyle, dietary habits, and even cultural beliefs about medication can lead to shared decision‑making that respects both evidence‑based medicine and personal agency. Additionally, while PPIs like omeprazole offer potent acid suppression, they bring concerns about bone health and nutrient absorption that must be weighed against the severity of a patient’s GERD symptoms, especially in older adults 👵👴. The takeaway, therefore, is not to dismiss alternative options outright but to engage in a nuanced conversation that weighs efficacy, safety, accessibility, and individual values. By fostering this inclusive dialogue, healthcare providers can help patients feel empowered rather than dictated to, which, in turn, often improves adherence and outcomes 📈. Ultimately, the goal remains the same: to alleviate discomfort, protect the gastrointestinal lining, and maintain overall well‑being, regardless of whether the chosen agent is famotidine, cimetidine, or a carefully managed PPI regimen. 🌟
jess belcher
October 15, 2025 AT 10:20When you need quick relief try famotidine it works fast and is easy on the wallet
Sophia Simone
October 15, 2025 AT 21:27It would be naïve to assume that famotidine universally supersedes all alternatives; the pharmacodynamic nuances of cimetidine, particularly its enzyme inhibition, render it indispensable in specific therapeutic niches, contrary to the oversimplified narratives widely propagated.
Juan Sarmiento
October 16, 2025 AT 08:34Exactly, Sophia! The reality is that each drug has its own spotlight, and for patients juggling multiple meds, the enzyme‑blocking property of cimetidine can actually protect against certain drug‑drug clashes, turning a perceived drawback into a strategic advantage. That’s why a personalized approach beats a blanket recommendation any day.
Cindy Knox
October 16, 2025 AT 19:40I’ve been on famotidine for months and my nightly heartburn has practically vanished, which feels like a small victory in my daily routine.
beverly judge
October 17, 2025 AT 06:47That’s great to hear, Cindy. For others experiencing similar symptoms, it can help to take famotidine an hour before dinner and avoid lying down immediately after meals; these small adjustments often enhance the medication’s effectiveness without any extra cost.
Capt Jack Sparrow
October 17, 2025 AT 17:54Just skip the H2 blockers and jump straight to a low‑dose PPI.
Manju priya
October 18, 2025 AT 05:00Embracing a new acid‑suppression plan can feel challenging, but remember that every small step toward better health builds momentum 😊. Choose a medication that aligns with your lifestyle, stay consistent, and celebrate each day you’re free from the burning discomfort that once held you back.
Jacqueline D Greenberg
October 18, 2025 AT 16:07I totally get how overwhelming the switch can be, and it’s okay to feel a little uneasy at first. Just keep a simple journal of what you eat, when you take your meds, and how you feel – that feedback loop can really demystify the process and make you feel more in control.
Jim MacMillan
October 19, 2025 AT 03:14While journaling is a charming habit, the real sophistication lies in periodic blood work to monitor B12 and magnesium levels when on PPIs; it’s the hallmark of a truly informed patient 💎.