Weight Loss Medication Recommender
This tool helps you match your specific health profile and weight-loss goals to the most appropriate prescription medications. Answer a few simple questions to see which options best fit your needs.
Find Your Best Weight-Loss Medication
Quick Takeaways
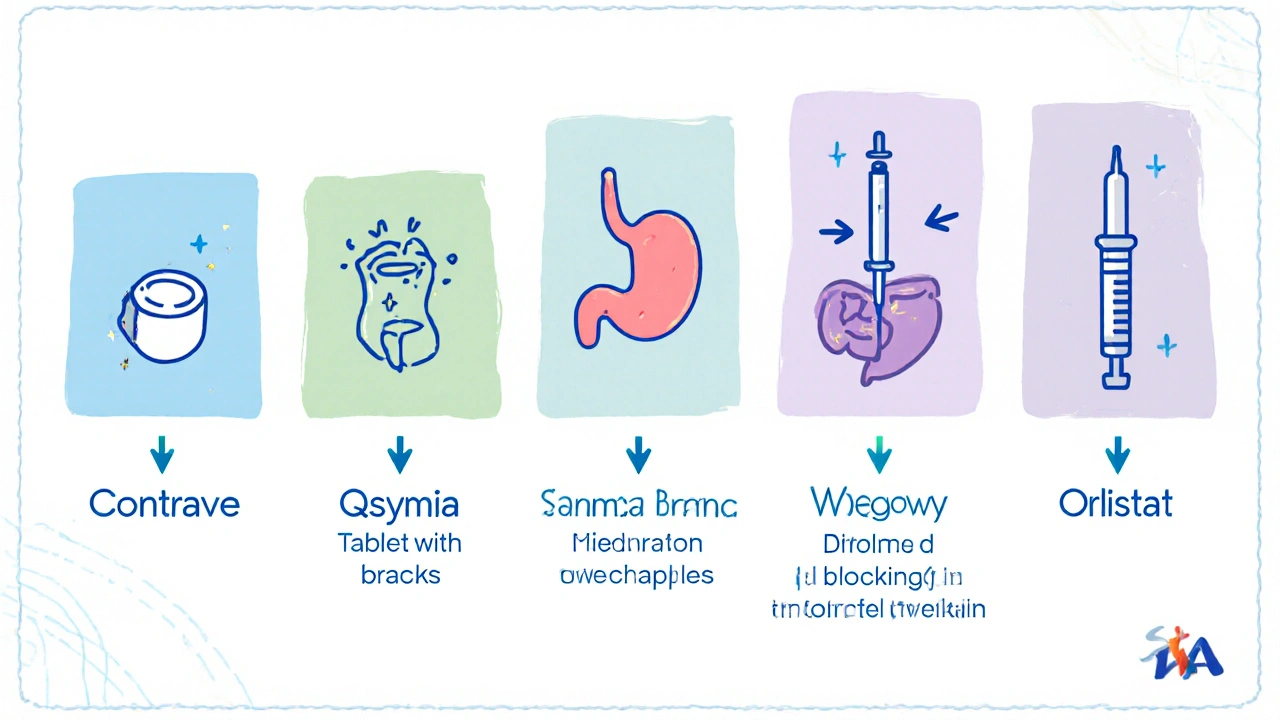
- Contrave combines naltrexone and bupropion to curb appetite and cravings.
- Qsymia (phentermine/topiramate) yields the highest average weight loss (10‑12%).
- Saxenda and Wegovy are injectable GLP‑1 agonists with strong safety records.
- Orlistat works locally in the gut and is the cheapest but offers modest results.
- Choosing the right drug depends on efficacy, side‑effect tolerance, cost, and insurance coverage.
If you’re hunting for a prescription that actually helps shed pounds, you’ve probably heard of Contrave - the oral combo of naltrexone and bupropion. But it isn’t the only player on the market. Below we break down how Contrave stacks up against the most popular alternatives, so you can decide which pill (or injection) fits your health goals and lifestyle.
What Is Contrave?
Contrave is a prescription medication approved by the FDA in 2014 for chronic weight management in adults with a BMI ≥30 or ≥27 with weight‑related conditions. It pairs two existing drugs: naltrexone, an opioid‑receptor antagonist, and bupropion, an atypical antidepressant that also reduces appetite.
How Contrave Works
The two ingredients hit different brain pathways. Naltrexone blocks the reward signals that trigger cravings, while bupropion stimulates the hypothalamus to boost feelings of satiety. The synergy is designed to curb both the urge to eat and the pleasure derived from food.
Key Benefits & Risks of Contrave
- Efficacy: Clinical trials report an average 5‑10% body‑weight reduction after one year.
- Convenience: Oral tablets taken twice daily - no injections.
- Safety profile: Most common side effects are nausea, constipation, and dry mouth. Rare but serious risks include increased blood pressure and mood changes.
- Contraindications: Not for patients with uncontrolled hypertension, seizure disorders, or a history of eating disorders.
Leading Alternatives
Below is a snapshot of the other FDA‑approved prescription options you’ll encounter when your doctor talks weight‑loss meds.
Qsymia blends phentermine (a stimulant) with topiramate (an anti‑seizure drug). It’s known for the highest average weight loss but carries a higher risk of insomnia and tingling sensations.
Saxenda is a daily injectable of liraglutide, a GLP‑1 receptor agonist originally used for type‑2 diabetes. It reduces appetite by slowing gastric emptying.
Wegovy contains semaglutide, another GLP‑1 agonist, but at a higher dose administered once‑weekly. Studies show up to 15% body‑weight loss in a year.
Phentermine/Topiramate (often called the “Qsymia combo”) works like a turbo‑charged appetite suppressant, but can raise heart rate and blood pressure.
Orlistat is a lipase inhibitor sold over‑the‑counter (brand name Xenical) that blocks about 30% of dietary fat absorption. It’s cheap and non‑systemic but can cause oily stools and flatulence.
Comparison Table
| Drug | Active ingredients | Mechanism | FDA approval year | Average % weight loss (12mo) | Typical side effects | Cost (US, monthly) |
|---|---|---|---|---|---|---|
| Contrave | Naltrexone+Bupropion | Reward‑pathway blockade + appetite‑satiety signaling | 2014 | 5‑10% | Nausea, constipation, dry mouth, ↑BP | $300‑$350 |
| Qsymia | Phentermine+Topiramate | Stimulant appetite suppression + neuro‑modulation | 2012 | 9‑12% | Insomnia, paresthesia, ↑heart rate | $250‑$300 |
| Saxenda | Liraglutide (GLP‑1 agonist) | Slows gastric emptying, enhances satiety | 2014 | 5‑8% | Nausea, vomiting, pancreatitis (rare) | $1,200‑$1,300 |
| Wegovy | Semaglutide (GLP‑1 agonist) | Same as Saxenda, but higher potency | 2021 | 12‑15% | Nausea, diarrhea, gallbladder disease (rare) | $1,350‑$1,500 |
| Orlistat | Orlistat | Lipase inhibition (blocks fat absorption) | 1999 (OTC 2007) | 2‑3% | Oily stools, flatulence, fat‑soluble vitamin deficiency | $30‑$50 |
How to Choose the Right Option
Use the following decision checklist to narrow down the best fit for you:
- Target weight‑loss goal: If you need >10% loss, GLP‑1 injectables (Wegovy) or Qsymia are most effective.
- Injection tolerance: Some patients dislike needles - Contrave, Qsymia, or Orlistat stay oral.
- Cardiovascular health: Avoid stimulant‑based combos (Qsymia, Phentermine) if you have hypertension.
- Side‑effect profile: If you’re prone to GI upset, Orlistat’s oily stools may be a deal‑breaker; GLP‑1 agents often cause nausea.
- Insurance coverage & cost: Oral pills (Contrave, Qsymia) usually have better formulary placement than pricey injectables.
- Underlying conditions: Diabetes patients may benefit from GLP‑1 drugs, which also improve glycemic control.
Discuss these points with your healthcare provider. They’ll weigh the clinical data against your medical history to prescribe the safest, most effective regimen.
Frequently Asked Questions
Can I take Contrave and another weight‑loss drug at the same time?
No. Combining prescription weight‑loss medications can increase the risk of serious side effects, especially blood‑pressure spikes. Your doctor should pick one agent that matches your profile.
How long should I stay on Contrave?
Most studies follow patients for 12 months. If you reach your weight goal and maintain it, a gradual taper is recommended under medical supervision.
Is Contrave safe for people with a history of depression?
Bupropion is actually an antidepressant, but it can also trigger mood swings in a minority of users. Close monitoring is essential if you have a psychiatric history.
Which drug loses the most weight?
Current head‑to‑head data show Wegovy (semaglutide) achieving the highest average loss-about 12‑15% of body weight in a year.
Do I need to follow a diet while taking these medications?
Yes. All prescription weight‑loss drugs are approved for use alongside a reduced‑calorie diet and increased physical activity. Meds alone rarely achieve long‑term success.
Weight‑loss pharmacotherapy is a powerful tool, but it works best when paired with sustainable lifestyle changes. Use this guide to compare Contrave with its main rivals and have a data‑driven conversation with your doctor.




Tiffany Owen-Ray
October 16, 2025 AT 16:43When you sit down to compare weight‑loss pharmacotherapies, the first thing to acknowledge is that each drug lives inside a unique neuro‑behavioral niche.
The dual‑action nature of Contrave, for example, attempts to tame both the hedonic reward circuit and the homeostatic hunger center, a synergy that few other agents aim for.
This synergy can feel like a philosophical compromise between desire and restraint, a sort of internal dialogue that mirrors the classic conflict between the id and the superego.
Yet the reality of clinical outcomes reminds us that no compound can rewrite biology without a price.
The average five‑to‑ten percent weight loss reported for Contrave emerges after a year of disciplined use, dietary adjustment, and regular activity.
By contrast, the GLP‑1 injectables such as Wegovy can push the number closer to fifteen percent, but they demand a weekly needle and a substantially higher financial commitment.
Qsymia occupies a middle ground, offering nine to twelve percent loss but bringing the stimulant side‑effects of phentermine into play, which may be intolerable for patients with cardiovascular concerns.
Orlistat, on the other hand, trades efficacy for affordability, siphoning off dietary fat at the cost of oily stools and vitamin supplementation.
The decision matrix, therefore, must balance efficacy, safety, cost, and personal lifestyle preferences.
If you value oral administration and are willing to monitor blood pressure, Contrave presents a viable compromise.
If your primary goal is rapid, substantial loss and you have insurance coverage for injectables, Wegovy may be the logical choice.
If you have a history of hypertension or anxiety, steering clear of stimulant‑based combos like Qsymia could protect your well‑being.
If finances are tight, the over‑the‑counter nature of Orlistat offers a modest benefit without breaking the bank.
Moreover, the psychological dimension cannot be ignored; some patients find the act of taking a daily pill a tangible reminder of their commitment, while others prefer the discreetness of a weekly shot.
Ultimately, a shared decision with your healthcare provider, grounded in these trade‑offs, will shape the path that feels both sustainable and ethically sound.
Remember, medication is a tool, not a magic wand, and its success hinges on the broader context of diet, movement, and self‑compassion.
Juan Sarmiento
October 19, 2025 AT 00:17I like how you broke down the pros and cons of each option. It really helps someone who’s overwhelmed by the sheer number of choices. For many folks, the oral route of Contrave or Qsymia feels less intimidating than a weekly injection. Pairing any of these meds with a realistic calorie deficit and regular walks makes the numbers in the table feel achievable. Keep the focus on sustainable habits, and the medication becomes a helpful sidekick rather than the main hero.
Jill Brock
October 21, 2025 AT 07:50Seriously, the pharmaceutical circus is out of control. They slap a price tag on a needle and call it a miracle while ignoring the nightmare side‑effects. If you’re not ready to gamble with your blood pressure, steer clear of those stimulant combos. Wake up and demand real lifestyle changes instead of hoping a pill does the heavy lifting.
Patrick McVicker
October 23, 2025 AT 15:23Orlistat is cheap but you’ll end up with greasy pizza nights.
Liliana Phera
October 25, 2025 AT 22:57Weight‑loss drugs are not a license to ignore the underlying behavioral patterns that drove the excess in the first place. The naltrexone component of Contrave tackles reward pathways, yet without addressing emotional eating, the relief is fleeting. If you keep feeding the same triggers, any pharmacologic aid will eventually wear thin. The temptation to view medication as a shortcut betrays a deeper denial of self‑responsibility. Challenge the narrative that a tablet can replace mindful nutrition. Only then will you truly harness the benefits each drug offers.
Poorni Joth
October 28, 2025 AT 05:30Honestly you cant just pop a pill and expect miracles it is morally wrong to rely on quick fixes that dont teach you discipline naltrexone bupropion may help but without a proper diet you are cheating yourself please read the fine print and dont blame the med for your own laziness.
Yareli Gonzalez
October 30, 2025 AT 13:03Your summary makes the options much clearer. I appreciate the balanced tone and the practical checklist. It’s a good reminder that medication should complement, not replace, lifestyle changes.
Alisa Hayes
November 1, 2025 AT 20:37The table provides a concise visual aid that many readers will find helpful. It succinctly captures efficacy, side‑effects, and cost in one glance. Maintaining this level of clarity throughout the thread will keep the discussion focused.
Mariana L Figueroa
November 4, 2025 AT 04:10Great job laying out the facts concisely Good info makes it easier to decide which option fits your budget and health goals Keep it up
Diane Helene Lalande
November 6, 2025 AT 11:43It’s reassuring to see a thorough overview that respects both the medical evidence and the personal preferences of patients. The inclusion of insurance considerations adds a realistic dimension that many guides overlook. Thank you for presenting the data without judgment.
Manju priya
November 8, 2025 AT 19:17Esteemed readers, consider this an invitation to approach weight management with both scientific rigor and disciplined commitment. The comparative analysis herein equips you to engage your physician in an informed dialogue. May your choice reflect a harmonious blend of efficacy, safety, and personal sustainability.
Jesse Groenendaal
November 11, 2025 AT 02:50People need to stop looking for shortcuts meds are not magic they require effort and discipline otherwise you waste money and health
Persephone McNair
November 13, 2025 AT 10:23The pharmacodynamic profiles delineated in the matrix underscore a mechanistic divergence: antagonism of µ‑opioid receptors versus GLP‑1 receptor agonism, each precipitating distinct homeostatic recalibrations. Accordingly, clinicians must stratify patients based on comorbidities, cardiovascular risk, and metabolic imperatives when selecting an agent.
siddharth singh
November 15, 2025 AT 17:57When evaluating anti‑obesity agents, it is essential to contextualize their mechanisms within the broader neuro‑endocrine circuitry governing energy balance.
Naltrexone, an opioid‑receptor antagonist, attenuates the dopaminergic reward signals that compel hedonic eating, while bupropion, a norepinephrine‑dopamine reuptake inhibitor, amplifies pro‑satiety pathways in the arcuate nucleus.
This dual action is theoretically advantageous because it simultaneously reduces the drive to consume palatable foods and enhances feelings of fullness.
Clinical trials have demonstrated a modest mean weight reduction of 5‑10 percent over twelve months, which, while statistically significant, may not satisfy patients seeking rapid results.
In contrast, GLP‑1 agonists such as semaglutide engage peripheral receptors to slow gastric emptying and central receptors to suppress appetite, often achieving double‑digit weight loss.
However, their injectable format and cost-exceeding a thousand dollars per month in many markets-pose barriers to widespread adoption.
The stimulant component of Qsymia, phentermine, raises basal metabolic rate and suppresses appetite via catecholamine release, but it also elevates heart rate and blood pressure, necessitating careful cardiovascular screening.
Orlistat's mechanism is confined to the gastrointestinal lumen, inhibiting pancreatic lipase and preventing absorption of approximately one third of ingested triglycerides, a mode of action that avoids systemic side‑effects but generates unpleasant oily stools.
Safety profiles must be weighed against efficacy; for instance, the rare risk of pancreatitis with liraglutide demands vigilance, whereas the most common adverse events across agents are gastrointestinal in nature.
Cost‑effectiveness analyses frequently reveal that oral agents like Contrave occupy a middle ground, offering reasonable efficacy without the financial burden of weekly injections.
Insurance formularies often prioritize older, generic options, which can influence prescribing patterns and patient adherence.
Moreover, patient preference regarding route of administration-pill versus injection-has been shown to affect long‑term compliance in multiple adherence studies.
Ultimately, the decision matrix should incorporate baseline BMI, comorbid conditions such as type‑2 diabetes or hypertension, and the individual's willingness to tolerate specific side‑effects.
Shared decision‑making, anchored in transparent discussion of these variables, empowers patients to select a therapy that aligns with their health goals and lifestyle constraints.
In summary, no single drug reigns supreme; the optimal choice emerges from a personalized synthesis of pharmacologic properties, clinical evidence, and patient‑centric considerations.
Angela Green
November 18, 2025 AT 01:30We should note that the original post contains several inconsistencies: “antagonist” is misspelled as “antagonst,” and “insulin‑resistance” should be hyphenated. Also, “the most effective” needs a comma after “however.” Finally, avoid using “its” when you mean “it’s.” Keeping the text grammatically pristine helps maintain credibility.