HIV Drug Interaction Checker
Check Medication Safety
When HIV was first identified, a diagnosis often meant a death sentence. Today, it’s a manageable condition - but only if the right medications are taken correctly. Antiretroviral therapy (ART) has turned HIV from a terminal illness into a chronic one, with people living near-normal lifespans when treatment is consistent. But behind that success lies a hidden battle: drug resistance and complex interactions that can undo years of progress. This isn’t theoretical. It’s happening in clinics, homes, and communities every day.
How Antiretroviral Drugs Work
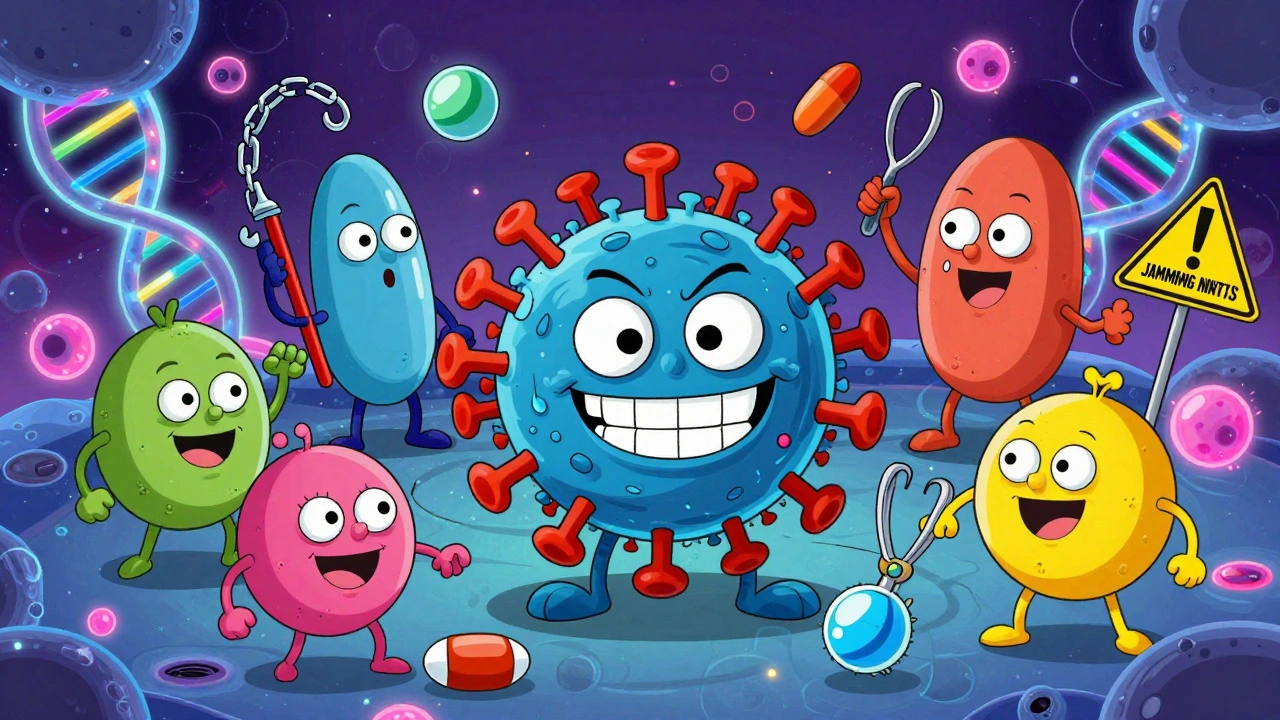
Antiretroviral medications don’t cure HIV. They stop it from multiplying. HIV needs to copy its genetic material to spread in the body. ART blocks that process at different stages. There are six main classes of drugs, each targeting a specific step in the virus’s life cycle.NRTIs like tenofovir and lamivudine act as fake building blocks. When HIV tries to copy its RNA, it grabs these imposters instead, and the chain breaks. NNRTIs like doravirine and efavirenz stick to the virus’s reverse transcriptase enzyme and jam it. PIs stop the virus from cutting its proteins into usable pieces. INSTIs - the most powerful class today - block HIV from inserting its DNA into human cells. Fusion inhibitors and CCR5 antagonists prevent the virus from even entering the cell.
Modern treatment almost always combines at least three drugs from two or more classes. Why? Because HIV mutates fast. One drug alone? The virus will adapt within weeks. But hitting it from multiple angles makes resistance harder to develop. That’s why first-line regimens today are usually two NRTIs plus an INSTI like dolutegravir or bictegravir. These combinations are simpler, safer, and more forgiving than older ones.
Why Drug Resistance Happens
Resistance isn’t magic. It’s evolution. Every time HIV copies itself, it makes mistakes. Most of these errors kill the virus. But sometimes, a mutation lets it survive even when drugs are present. If you miss doses, drug levels drop. That gives resistant strains room to grow.Some mutations are common and predictable. The M184V mutation makes HIV resistant to lamivudine and emtricitabine - two of the most widely used NRTIs. The K65R mutation weakens tenofovir. For NNRTIs, a single K103N mutation can knock out efavirenz and nevirapine. But INSTIs like dolutegravir are tougher. They need multiple mutations to lose effectiveness. That’s why they’re now the gold standard.
But resistance isn’t just about missed pills. It can be transmitted. About 1 in 6 newly diagnosed people in the U.S. already have HIV that’s resistant to at least one drug. That’s why genotype testing is required at diagnosis. Without it, you might start a regimen that’s already useless.
Drug Interactions: The Silent Threat
Most people with HIV aren’t just taking antiretrovirals. They’re also on meds for high blood pressure, cholesterol, depression, or diabetes. That’s where things get dangerous.Boosted protease inhibitors - like darunavir with ritonavir or cobicistat - are strong inhibitors of liver enzymes (CYP3A4). They can cause other drugs to build up to toxic levels. Simvastatin, a common cholesterol drug, becomes deadly when taken with boosted PIs. Midazolam, used for sedation, can cause prolonged coma. Even over-the-counter supplements like St. John’s wort can drop ART levels enough to trigger resistance.
Even newer drugs aren’t immune. Doravirine has fewer interactions than efavirenz, but it still reacts with some antifungals and seizure meds. Tenofovir alafenamide (TAF) is gentler on kidneys than its older cousin TDF, but it still needs monitoring if you’re on other nephrotoxic drugs.
There are over 100 known drug interactions with ART. The Liverpool HIV Interactions Database is the go-to tool for clinicians - but not every provider has time to check it. That’s why many patients end up on unsafe combinations. A 2024 study found nearly half of people with HIV take five or more non-HIV medications. That’s a recipe for disaster if not managed carefully.
What Happens When Resistance Strikes
Viral rebound - when the virus starts multiplying again - is the first sign something’s wrong. It’s often silent. No fever. No rash. Just a rising viral load on routine blood tests. That’s why regular monitoring is non-negotiable.If resistance is confirmed, the old regimen is scrapped. The next step? A resistance test. Not just any test - a full genotype. It shows exactly which mutations are present. Then, using tools like the Stanford HIVdb algorithm, doctors figure out which drugs still work.
Salvage therapy used to mean stacking five or six drugs. Now, it’s smarter. For multi-drug resistant cases, dolutegravir plus boosted darunavir works in over 90% of cases. But even that’s changing. A new drug, VH-184, showed promise in early trials, suppressing HIV strains that resisted dolutegravir and bictegravir. It’s not yet approved, but it’s a sign that resistance is being outmaneuvered, not just endured.
Long-Acting Injections: Hope and Risk
For many, daily pills are a burden. That’s why long-acting injectables like Cabenuva (cabotegravir plus rilpivirine) are a game-changer. One shot every month - or even every two months - replaces a pillbox. In trials, 94% of users preferred injections. Adherence jumped. Viral suppression stayed high.But here’s the catch: if you miss an injection, the drug levels drop slowly. For weeks, you’re in a gray zone - enough drug to suppress the virus a little, but not enough to stop resistance. That’s why experts warn: long-acting doesn’t mean forgiving. One missed dose can set you back months.
Lenacapavir, approved in 2022 and now recommended for prevention by WHO, works even longer - every six months. But its use is limited to people with heavily resistant HIV. It’s not for beginners. And if it fails? There are few backups.
Who’s at Risk - and How to Stay Safe
Anyone who skips doses is at risk. But some face higher danger. People with mental health conditions, unstable housing, or substance use disorders struggle with adherence. Older adults on multiple meds are more likely to have interactions. Those in rural areas may not get timely resistance testing - delays of three weeks or more are common.Prevention isn’t immune either. Truvada and Descovy as PrEP are highly effective - but only if taken daily. There are documented cases of people acquiring resistant HIV while on PrEP. The M184V mutation showed up in one case after a person missed doses during a weekend binge. That’s why PrEP isn’t a magic shield. It’s a tool - and tools fail if misused.
The best defense? Consistency. Use pill organizers. Set phone alarms. Link meds to daily routines - brushing teeth, eating breakfast. If side effects hit - insomnia from efavirenz, nausea from tenofovir - talk to your provider. Don’t quit. There are alternatives. Dolutegravir-based regimens like Biktarvy have fewer side effects and higher adherence rates.
Tools and Resources You Can Use
You don’t have to navigate this alone. The NIH’s HIV Drug Interaction Checker lets you plug in your meds and see red flags. The Johns Hopkins HIV Guide app is free and used by over 285,000 people. It includes resistance patterns, dosing, and interaction alerts.For providers, training matters. Community clinics often lack specialists. A 2024 study showed only 85% of non-specialists correctly interpret resistance reports. That’s why tools like the IAS-USA guidelines - rated 4.7 out of 5 for clarity - are so vital. They cut through the noise.
And don’t underestimate support. Reddit’s r/HIV community has over 12,000 members sharing real stories - missed doses, side effects, breakthroughs. Hearing someone else say, “I went through this too,” can be the difference between quitting and sticking with treatment.
The Future: AI, Gene Editing, and Beyond
The next wave isn’t just better drugs - it’s smarter care. AI tools like HIV-TRACE can predict which strains are spreading in a community by analyzing genetic sequences. That helps public health teams target interventions before resistance becomes widespread.Researchers are also exploring CRISPR gene editing to cut HIV DNA out of infected cells. Early animal studies show 95% reduction in viral DNA. It’s not ready for humans yet - but it’s a glimpse of a future where HIV isn’t managed, but erased.
For now, the goal is simple: suppress the virus, avoid resistance, prevent interactions. Every pill taken on time is a victory. Every interaction checked is a saved life. The science has come far. But the human part - remembering, asking, staying connected - is still the most powerful drug we have.

Louis Llaine
December 8, 2025 AT 04:09So let me get this straight - we’ve turned HIV into a chronic condition, but only if you’re rich, stable, and have a personal assistant to remind you to take your pills? Cool. I’m sure the guy sleeping under the bridge with three other meds and no phone is just thrilled.
Also, ‘dolutegravir is the gold standard’ - sure, until your insurance drops it next year and you’re stuck with efavirenz again. Thanks for the optimism, doc.
And don’t even get me started on ‘long-acting injections.’ Yeah, great. Miss one shot and now you’re breeding super-virus while your provider’s on vacation. Real safe.
Meanwhile, Big Pharma’s laughing all the way to the bank. $2000/month for a pill that works… if you don’t skip it. Classic.
Sam Mathew Cheriyan
December 9, 2025 AT 12:34haha ok but what if the virus is actually a government bioweapon and the meds are just keeping us docile? i mean why do they say 'no cure' but give us drugs for life? and why do they never talk about the 7 other viruses they say are 'controlled' but never cured? also st johns wort is banned in 12 countries for a reason lol
my cousin in delhi took arv and now he can levitate? not joking. i saw it on youtube. maybe the drugs are opening the third eye? 🤔
Ernie Blevins
December 10, 2025 AT 14:35Everyone’s acting like this is a medical breakthrough. Nah. This is a money machine. You think people with HIV want to take pills forever? No. They want to be cured. But cures don’t make recurring revenue.
Look at the stats - 1 in 6 new cases already have resistance? That’s not bad luck. That’s systemic failure. And the ‘solution’? More expensive drugs. More testing. More co-pays.
They’re not fighting HIV. They’re farming it. And you’re all just clicking ‘agree’ on the consent form while they bill your insurance for $12,000 a year. Wake up.
Jennifer Anderson
December 12, 2025 AT 01:41Just wanted to say - if you’re reading this and you’re struggling with adherence, you’re not alone. I missed doses for months after my mom passed. Felt like a failure.
Then I started linking my meds to my morning coffee. Set a dumb alarm that plays my favorite song. Talked to my pharmacist - she gave me a pillbox with colors.
It’s not perfect. Some days I still forget. But I keep trying. And that’s enough.
You’re not broken. You’re human. And you deserve to live.
Also - if you’re on PrEP and you’re scared you missed a dose? Call your clinic. Don’t panic. We’ve got your back.
Oliver Damon
December 13, 2025 AT 18:12The evolutionary dynamics of HIV resistance represent a quintessential case study in viral adaptive selection under pharmacological pressure. The selective sweep of mutations such as M184V and K65R reflects a fitness landscape modulated by subtherapeutic drug concentrations - essentially, a Darwinian arms race occurring within the intracellular milieu.
What’s underappreciated is the epistatic interactions between resistance mutations. For instance, K65R + M184V creates a compensatory fitness cost that paradoxically increases susceptibility to zidovudine - a phenomenon known as resensitization.
Furthermore, the pharmacokinetic-pharmacodynamic (PK-PD) disconnect between long-acting injectables and viral rebound kinetics introduces a novel therapeutic window challenge: subtherapeutic troughs without overt clinical symptoms enable cryptic replication. This necessitates a paradigm shift from adherence metrics to pharmacokinetic monitoring via dried blood spot assays.
The real bottleneck isn’t drug development - it’s implementation fidelity in resource-constrained settings. We need decentralized resistance testing infrastructure, not just better drugs.
Kurt Russell
December 14, 2025 AT 11:26YOU ARE NOT ALONE. I’ve been on ART for 17 years. I’ve had viral rebounds. I’ve cried in my car after missing a dose. I’ve been scared. But I’m still here.
And guess what? So can you.
Find your person. Your support group. Your Reddit thread. Your pharmacist who remembers your name. Your doctor who doesn’t judge.
One pill. One shot. One day at a time. That’s how we win.
And if you think long-acting injections are risky? Try living with a viral load you can’t control. That’s the real risk.
You got this. I believe in you. Now go take that pill. I’m cheering for you.
Kyle Flores
December 16, 2025 AT 04:09Just wanted to add - if you’re on meds and you’re scared to tell your family or partner? You don’t have to. But if you’re ready? There are people who will hold space for you.
I used to hide my pillbox. Now I keep it next to my toothbrush. My partner knows what it is. We don’t talk about it every day - but when we do, it’s not shame. It’s care.
Also - if you’re a provider reading this? Don’t assume someone’s non-adherent because they’re poor or busy. Ask them what’s getting in the way. Then shut up and listen.
This isn’t just science. It’s human.
Ryan Sullivan
December 16, 2025 AT 08:41It is a matter of profound institutional negligence that the medical establishment continues to rely on patient compliance as the primary mechanism of viral suppression. The very premise of ART as a lifelong regimen - predicated on behavioral fidelity - is an archaic model in an age of precision pharmacology.
The failure to implement mandatory, real-time pharmacokinetic monitoring for all patients on long-acting regimens constitutes a breach of the standard of care. Furthermore, the normalization of ‘resistance as inevitable’ reflects a dangerous complacency that prioritizes cost containment over clinical sovereignty.
The emergence of VH-184 is not a breakthrough - it is a belated correction. We should have been here a decade ago. The fact that we are not speaks volumes about the moral economy of pharmaceutical innovation.
Until we decouple treatment access from socioeconomic status, we are not treating disease - we are rationing survival.