Antibiotic Choice Decision Tool
Recommended Treatment
When a clinician reaches for Chloramycetin alternatives, the decision isn’t just about picking any pill. The drug’s historic reputation, broad‑spectrum activity, and notorious safety concerns make it a tricky choice. Below you’ll find a plain‑English rundown of what Chloramphenicol actually does, why you might want something else, and a side‑by‑side look at the most common substitutes.
What is Chloramphenicol (Chloromycetin)?
Chloramphenicol is a synthetic broad‑spectrum antibiotic that inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit. First marketed as Chloromycetin in the late 1940s, it quickly earned a place in the treatment of serious infections like typhoid fever, meningitis, and anaerobic intra‑abdominal infections.
Its strength lies in tackling both Gram‑positive and Gram‑negative organisms, including some that shrug off newer drugs. However, the price of that versatility is its association with rare but life‑threatening bone‑marrow suppression (aplastic anemia) and dose‑related gray‑baby syndrome in newborns.
Why Look for Alternatives?
Three practical reasons push clinicians toward other agents:
- Safety profile - The risk of irreversible blood‑cell loss outweighs the benefit for most routine infections.
- Resistance trends - Many regions report rising chloramphenicol‑resistant strains, especially in urinary‑tract and respiratory pathogens.
- Guideline alignment - Modern treatment protocols (IDSA, WHO) rarely list chloramphenicol as first‑line, preferring agents with clearer efficacy data.
Understanding the trade‑offs helps you choose an alternative that matches the infection type, patient age, and safety considerations.
Head‑to‑Head Comparison Table
| Antibiotic | Typical Spectrum | Common Indications | Usual Dosage (Adult) | Major Side Effects | Resistance Risk |
|---|---|---|---|---|---|
| Chloramphenicol | Broad (Gram‑+, Gram‑‑, anaerobes) | Typhoid, meningitis, anaerobic infections | 500mg PO q6h | Aplastic anemia, gray‑baby syndrome | Moderate, especially in E.coli |
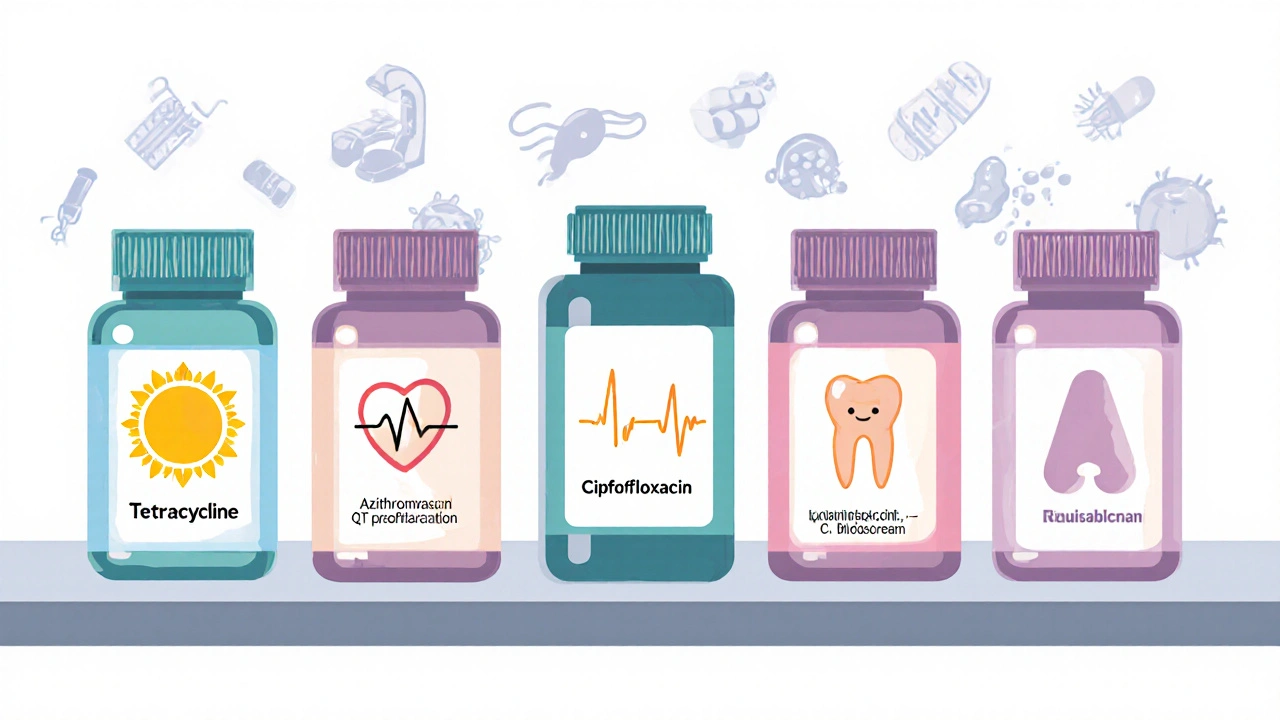
| Tetracycline | Broad (incl. atypicals) | Acne, rickettsial disease, chlamydia | 500mg PO q6h | Photosensitivity, teeth discoloration (kids) | Low to moderate |
| Azithromycin | Gram‑+, Gram‑‑, atypicals | Respiratory infections, STIs, traveler's diarrhea | 500mg PO daily ×3days | GI upset, QT prolongation | Low |
| Ciprofloxacin | Gram‑‑ (Pseudomonas), some Gram‑+ | UTI, abdominal sepsis, bone‑joint infections | 500mg PO BID | Tendon rupture, CNS effects | Moderate |
| Amoxicillin | Gram‑+ (Streptococcus), some Gram‑‑ | Otitis media, sinusitis, pneumonia | 875mg PO q12h | Allergic rash, GI upset | Low |
| Clindamycin | Gram‑+ (Anaerobes), some Gram‑‑ | Skin & soft‑tissue, intra‑abdominal, bone infections | 600mg PO q8h | Clostridioides difficile colitis | Low |
Deep Dive into Each Alternative
1. Tetracycline
Tetracycline is a broad‑spectrum, bacteriostatic drug that blocks the 30S ribosomal subunit, halting protein synthesis.
It shines in treating atypical organisms like Rickettsia and Mycoplasma. Its biggest drawback is photosensitivity - patients need to avoid strong sunlight for a week after dosing.
2. Azithromycin
Azithromycin belongs to the macrolide class and binds to the 50S ribosomal subunit, offering a long half‑life that supports short‑course regimens.
Because it concentrates in immune cells, it works well for intracellular pathogens. The main safety note is QT prolongation, so caution with patients on anti‑arrhythmics.
3. Ciprofloxacin
Ciprofloxacin is a fluoroquinolone that inhibits DNA gyrase and topoisomerase IV, leading to bacterial DNA damage.
Its strength is activity against Pseudomonas and many Gram‑negative rods, making it a go‑to for complicated UTIs. Tendon‑rupture warnings, especially in older adults, limit its use for uncomplicated infections.
4. Amoxicillin
Amoxicillin is a beta‑lactam penicillin that stops cell‑wall synthesis by binding penicillin‑binding proteins.
Widely tolerated, it’s first‑line for ear infections and many community‑acquired pneumonias. The main concern is allergic reactions in patients with penicillin hypersensitivity.
5. Clindamycin
Clindamycin is a lincosamide that also targets the 50S ribosomal subunit, providing good coverage of anaerobic bacteria.
It’s a strong choice for skin‑and‑soft‑tissue infections where anaerobes are suspected. The trade‑off is a marked risk of C.difficile-associated diarrhea, so it should be reserved for cases where alternatives fail.

How to Pick the Right Substitute
Use this three‑step decision tree:
- Identify the pathogen type. If you’re dealing with a known Gram‑negative rod, ciprofloxacin or amoxicillin‑clavulanate may be preferable. For anaerobes, clindamycin steps in.
- Assess patient factors. Age, pregnancy status, renal function, and allergy history can instantly rule out options. For example, avoid tetracycline in children under 8.
- Match safety to severity. In life‑threatening meningitis, the broad reach of chloramphenicol might still be justified, but for uncomplicated sinusitis a short course of amoxicillin is safer.
When in doubt, check local antibiograms - they give real‑world resistance patterns that can tilt the balance.
Practical Checklist for Clinicians
- Confirm organism susceptibility (culture or rapid PCR).
- Screen for drug allergies (especially penicillins, macrolides).
- Review renal and hepatic function; adjust doses for eGFR<30mL/min.
- Consider pregnancy or lactation - avoid tetracycline and chloramphenicol.
- Educate patients on side‑effect red flags (e.g., unexplained bruising → possible aplastic anemia).
- Document the reason for choosing an alternative (guideline deviation, resistance, safety).
Frequently Asked Questions
Is chloramphenicol still used in modern medicine?
Yes, but only for specific indications where its broad spectrum outweighs safety concerns - for example, meningitis caused by Haemophilus influenzae in regions with high resistance to beta‑lactams.
What is the most common serious side effect of chloramphenicol?
Aplastic anemia, a rare but irreversible bone‑marrow failure that can occur unpredictably even after short courses.
When should I choose azithromycin over amoxicillin?
If the infection is likely caused by atypical organisms (e.g., *Mycoplasma pneumoniae*) or if the patient is allergic to penicillins, azithromycin is a better fit.
Can I use ciprofloxacin for a simple urinary tract infection?
It works, but guidelines usually recommend nitrofurantoin or trimethoprim‑sulfamethoxazole first because fluoroquinolones carry higher risks of tendon injury and promote resistance.
What monitoring is needed if I must prescribe chloramphenicol?
Baseline complete blood count (CBC) before starting, then weekly CBC for the first month. Stop the drug immediately if white‑cell or platelet counts drop.
Choosing the right antibiotic is never a one‑size‑fits‑all decision. By weighing spectrum, safety, local resistance, and patient specifics, you can move beyond chloramphenicol and land on a drug that treats the infection efficiently while keeping side‑effects in check.




Sadie Bell
October 8, 2025 AT 14:34Alright folks, if you’re juggling infection types and patient allergies, start by nailing down the pathogen. The tool’s dropdowns make that a breeze, so don’t overthink it. Once you have the basics, the recommended antibiotic usually falls right out of the list. Keep the patient’s age in mind-kids and the elderly need gentler choices.
Noah Bentley
October 10, 2025 AT 22:07The description of chloramphenicol’s side‑effects uses the phrase “dose‑related gray‑baby syndrome”, but “dose‑related” is redundant; we already know it’s dose‑dependent. Also, “broad (Gram+, Gram‑, anaerobes)” could be cleaner-just say “broad‑spectrum covering Gram‑positive, Gram‑negative and anaerobes”.
Kathryn Jabek
October 13, 2025 AT 00:07In deliberating antimicrobial therapy, one must weigh pharmacodynamic potency against toxicity profiles. Chloramphenicol, while historically pivotal, carries an inherent risk of irreversible marrow suppression that dwarfs its spectrum advantage. Contemporary guidelines therefore prioritize agents with a more favorable safety margin, reserving chloramphenicol for select, refractory cases. The comparative table succinctly illustrates that macrolides and penicillins achieve comparable coverage with substantially lower adverse event rates. Accordingly, a judicious clinician will circuitously navigate toward these alternatives before contemplating chloramphenicol.
Ogah John
October 14, 2025 AT 17:47Ah, the allure of a “one‑size‑fits‑all” drug is as tempting as it is naïve. If you enjoy flirting with fatal bone‑marrow loss, go ahead; otherwise, let the data guide you. Remember, the most “broad” antibiotic is only as good as the patient’s tolerance for its side‑effects.
Kelvin Murigi
October 16, 2025 AT 03:07Chloramphenicol's broad spectrum is tempting, but the marrow toxicity can't be ignored. In practice, most clinicians reserve it for life‑threatening infections where alternatives truly fail. The drug penetrates the cerebrospinal fluid well, which is why it still appears in meningitis protocols in low‑resource settings. However, the risk of aplastic anemia, though rare, is essentially unpredictable and often irreversible. When you weigh that against a well‑tolerated beta‑lactam like amoxicillin, the balance tips dramatically. Moreover, resistance patterns have shifted; many Enterobacteriaceae now carry chloramphenicol‑acetyltransferase enzymes that blunt its efficacy. For uncomplicated urinary‑tract infections, a short course of ciprofloxacin or nitrofurantoin delivers cure rates above 90 % with far fewer safety concerns. If you suspect anaerobic involvement, clindamycin offers reliable coverage and a far more manageable side‑effect profile. In dermatologic indications such as severe acne, tetracycline or doxycycline remain first‑line because they avoid the hematologic hazards entirely. Travelers heading to endemic typhoid zones should consider azithromycin as a pragmatic alternative-its single‑dose regimen simplifies adherence. Pediatric patients under eight cannot receive tetracycline or fluoroquinolones, making azithromycin or amoxicillin the safest bets. For patients with penicillin allergy, clindamycin fills the gap without invoking the QT prolongation seen with macrolides. Always check local antibiograms before defaulting to a broad agent; data often reveal that a narrower drug will succeed. Dosing adjustments for renal impairment are straightforward for most oral agents, whereas chloramphenicol requires meticulous monitoring. In short, reserve chloramphenicol for cases where its unique pharmacokinetics are indispensable, and otherwise opt for a safer, guideline‑endorsed alternative.
ahmad matt
October 17, 2025 AT 06:54Looks like you forgot chloramphenicol is a last resort not a first‑line choice its toxicity makes it unsuitable for routine infections
kristine ayroso
October 18, 2025 AT 05:07Hey everyone, love how this post breaks down the options! It’s super helpful to see the side‑effects laid out in plain language. I especially appreciate the reminder about kids and tetracycline – so many people miss that detail.
Ben Small
October 18, 2025 AT 21:47Pick the safest drug that still covers the bug.
Dylan Hilton
October 19, 2025 AT 11:41Great breakdown; the decision tree really simplifies the choice. Just remember to double‑check local resistance patterns before finalizing.
Christian Andrabado
October 19, 2025 AT 22:47Nice summary – stick to guidelines.
Chidi Anslem
October 20, 2025 AT 07:07In summary, chloramphenicol remains a valuable tool in the antimicrobial arsenal when no better options exist. Its broad coverage can be lifesaving in severe infections, yet the safety concerns demand careful patient selection. Use the decision tool to match pathogen, patient factors, and local susceptibility. This approach ensures both efficacy and safety in modern practice.