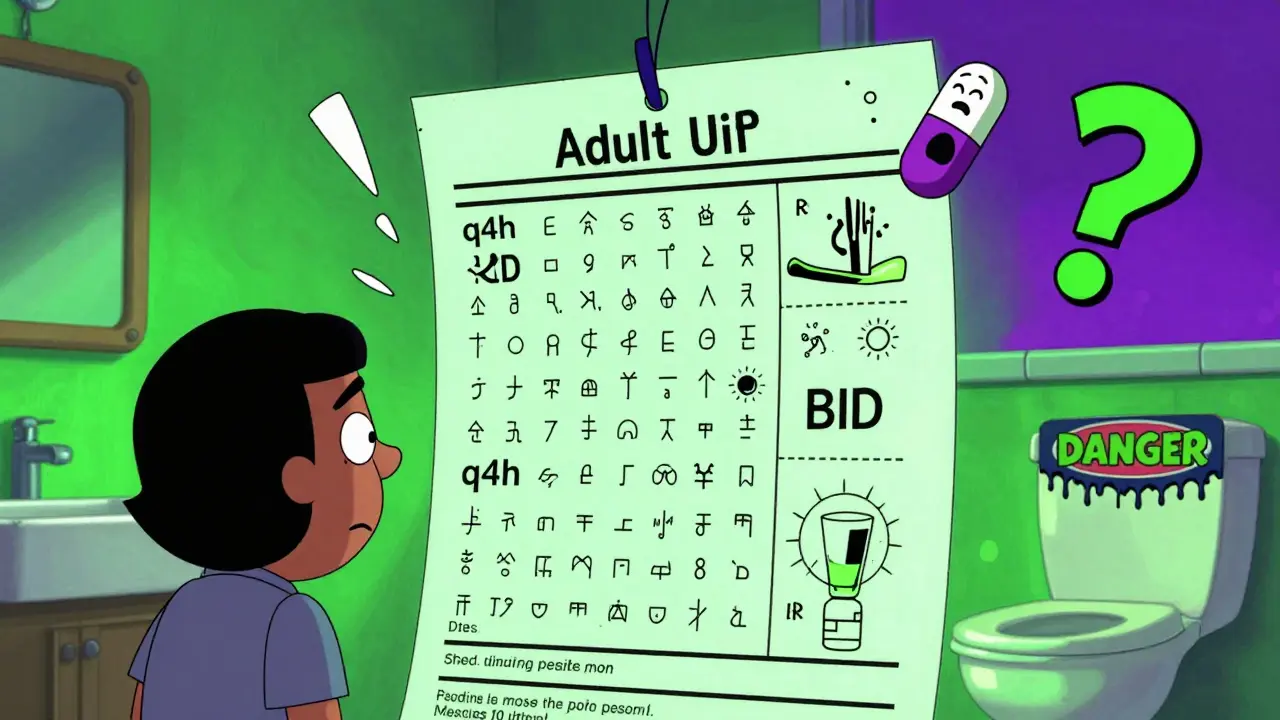
Every year, millions of people take their medicine the wrong way-not because they’re careless, but because the label doesn’t make sense. You’ve probably seen it: tiny text, weird abbreviations like "q4h" or "BID," and symbols that look like hieroglyphs. If you’ve ever stared at your prescription bottle wondering if "take twice daily" means every 12 hours or just morning and night, you’re not alone. And you’re not the only one who’s taken too much-or too little-because of it.
What’s Really on the Label?
Prescription labels aren’t just instructions. They’re safety tools. But too often, they’re written for pharmacists, not patients. The average prescription label uses language that’s harder to read than a college textbook. Studies show 27% of instructions are written at a reading level above high school. That means if you didn’t finish high school-or even if you did, but haven’t read much since-you’re already at a disadvantage.Common mistakes? "Take every 4-6 hours" gets confused with "take four times a day." People think "take with food" means eat something right before popping the pill, not that the pill should be swallowed during or right after a meal. Some patients skip doses because they think "once daily" means "once total," not every day. One Reddit user shared how they took their antibiotic four times a day for three days thinking "q6h" meant four times because 24 divided by 6 equals 4. They ended up in the ER with stomach bleeding.
And it’s not just words. Symbols matter too. The FDA tested common icons-like a fork for "take with food" or a glass of water for "take with fluids." Over 68% of people got them wrong. One icon that looks like a sun might mean "take in the morning," but another patient thinks it means "take during daylight hours." No wonder confusion is so common.
Who’s Most at Risk?
It’s easy to assume only older adults or people with low education are affected. But the truth is more complicated. A 2009 study found that even college-educated adults misread instructions 23% of the time. Why? Because the language is designed poorly, not because the person is unintelligent.Older adults (65+) are especially vulnerable. One in three seniors skip or change doses because the instructions don’t make sense. Spanish-speaking patients face even bigger hurdles. Only 12% of U.S. pharmacies offer labels in Spanish-even though over 41 million Americans speak it at home. And when translations are provided, they’re often literal, not clear. "Tomar una pastilla dos veces al día" might be grammatically correct, but if the patient doesn’t know what "pastilla" means, or if "dos veces" is misinterpreted as "two pills," the risk goes up.
People with memory issues, dementia, or cognitive decline are at the highest risk. Even with perfectly clear labels, misunderstanding rates stay above 60% in this group. That’s why tools like pill organizers and smartphone reminders are so common-78% of users create their own systems just to stay safe.
How Labels Should Be Designed
There’s a better way. Experts agree: clear labels use simple language, active voice, and visual cues. Instead of "Take one tablet by mouth twice daily," the best labels say: "Take 1 tablet by mouth two times each day-once in the morning and once at night."Here’s what works:
- Use full words: Write "daily," not "QD." Write "two times," not "BID." Write "at bedtime," not "qHS."
- Use active voice: "Take the pill" instead of "The pill should be taken."
- Limit steps: One instruction per line. No more than two steps total.
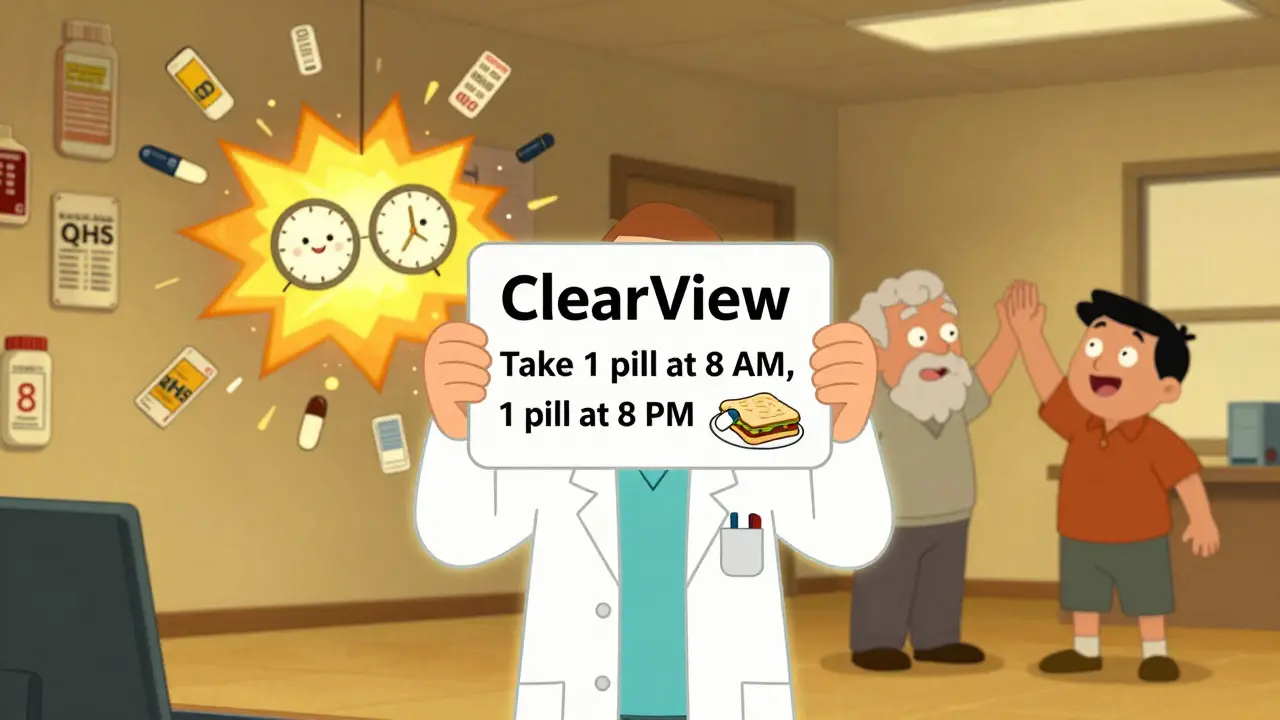
- Use clocks: Add a simple drawing of a clock showing 8 AM and 8 PM for twice-daily meds.
- Use icons wisely: Only use FDA-approved symbols, and test them with real patients first.
- Keep reading level at 6th grade or lower: That’s the standard recommended by the FDA and USP.
Pharmacies like CVS and Walgreens have started using these standards under their "ClearView" and "EasyRead" label systems. In one 2018 study, patients understood these labels 31% better than those from independent pharmacies still using old templates.
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s what you can do the next time you pick up a prescription:- Ask the pharmacist to explain it out loud. Don’t just take the label and leave. Say: "Can you tell me exactly when and how to take this?"
- Use the teach-back method. After they explain, say: "So, just to make sure I got it-I take one pill at 8 a.m. and another at 8 p.m., right?" If they nod, you’re good. If they hesitate, ask again.
- Request large-print labels. Almost all major pharmacy chains (CVS, Walgreens, Walmart) offer them for free. Just ask.
- Ask for visual aids. Can they add a clock icon? A simple drawing of a meal with a pill next to it? Many pharmacies will do it if you ask.
- Take a photo of the label. Use your phone to snap a picture. Then, use an app like GoodRx’s "Label Lens"-it scans the label and rewrites it in plain language.
- Write it down. Even if you’re tech-savvy, write the instructions on a sticky note and put it on your fridge or bathroom mirror.
What Pharmacies Need to Change
Pharmacists aren’t the problem-they’re overworked and under-supported. The real issue is outdated systems. Many pharmacy software platforms (like Epic, Cerner, and Rx30) generate labels with different fonts, sizes, and layouts. One pharmacy might use 14-point bold text. Another might use 10-point gray text. The contrast can be so poor, it’s hard to read even for people with perfect vision.There’s a solution: USP Chapter <17>. It’s a set of national standards for prescription labels that include:
- Drug name in large, bold font (minimum 12pt)
- Dosage instructions in plain language
- Standardized warning icons (approved by the FDA)
- Reading level no higher than 6th grade
Forty-two states have adopted these standards-but they’re not required by law. That means a pharmacy in one town might follow them, while the one across the street doesn’t. Independent pharmacies often skip upgrades because updating software costs $2,500-$5,000 per location. Chain pharmacies, with more resources, have moved faster.
But change is coming. In 2025, new rules will require QR codes on labels that link to video instructions in multiple languages. Early tests at Mayo Clinic showed a 62% drop in errors. The Biden administration has also pledged $200 million to improve health literacy by 2026. And Amazon Pharmacy just launched voice-enabled labels that read instructions aloud-cutting senior errors by 38% in trials.
Why This Matters More Than You Think
Misreading a label isn’t just inconvenient. It’s dangerous. In the U.S., medication errors from unclear labels cause:- 1.3 million emergency room visits every year
- Over 350,000 hospital admissions
- An estimated $200 billion in avoidable healthcare costs
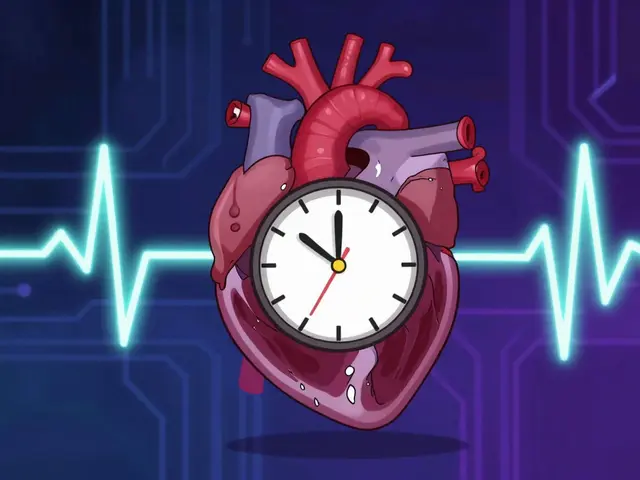
That’s not just money. It’s lives. A patient who takes too much blood pressure medicine can collapse. Someone who skips antibiotics can develop a deadly infection. A senior who takes their pill twice by accident might end up in the hospital with internal bleeding.
And here’s the hard truth: even if you’re healthy, educated, and careful, you can still be fooled. The system is broken. Labels are designed by people who don’t understand how patients actually read them. Until that changes, we all need to be our own safety net.
Final Tip: Don’t Assume Anything
Never guess. Never assume. If the label says "take with food," and you’re not sure what that means, ask. If it says "take every 8 hours," and you’re not sure if that’s 8 a.m., 4 p.m., and midnight-or just three times a day-ask. If the font is too small, ask for a larger version. If the instructions are confusing, ask for a diagram.There’s no shame in asking. In fact, the best patients are the ones who ask. And the best pharmacists? They don’t just hand you a bottle. They make sure you walk away knowing exactly what to do with it.


Lana Kabulova
January 22, 2026 AT 08:45Okay but why is it still acceptable for pharmacies to use 'BID' and 'QD'? I had a friend take her blood thinner twice in one day because she thought 'BID' meant 'before bedtime'-and she had a biochemistry degree. This isn't about literacy-it's about lazy design. We wouldn't let a car manual use hieroglyphs, so why do this with life-saving meds?
Chiraghuddin Qureshi
January 22, 2026 AT 10:37Same in India 😅 We have 'twice a day' written in Hindi but people still take it at 6am and 6pm instead of 12h apart. And the icons? One guy thought the 🍽️ meant 'eat after taking pill' not 'take with food'. We need voice labels. Or AI that yells at you if you open the bottle at the wrong time 🤣
Ryan Riesterer
January 22, 2026 AT 10:38The underlying issue is systemic: pharmacy information systems are legacy, siloed, and optimized for billing workflows-not patient comprehension. The FDA’s 6th-grade reading level guideline is empirically sound, yet adoption remains voluntary. The cost-benefit analysis for independent pharmacies favors risk externalization over compliance. Until reimbursement models incentivize clear labeling, this will persist as a structural failure.
Jasmine Bryant
January 23, 2026 AT 10:42I didn't know Walmart does free large print labels!! I've been squinting at mine for years. Just asked my pharmacist last week and she printed me a giant version with a little clock drawn next to 'take at night'. Best 30 seconds of my life. You guys should ask. Seriously. They're not gonna say no. 😅
Liberty C
January 24, 2026 AT 06:17It’s not that labels are confusing-it’s that people refuse to read them. I’ve seen patients hold up a bottle and say 'I don’t know what this says' while wearing reading glasses. The problem isn’t the label. It’s the refusal to engage with basic responsibility. If you can’t read 'take two times a day,' maybe you shouldn’t be managing your own meds. Stop blaming the system and start taking ownership.
Margaret Khaemba
January 26, 2026 AT 03:55My grandma uses a pill organizer with alarms and she still forgets sometimes. But the one thing that helped? When the pharmacist wrote 'Take with breakfast' and drew a little egg next to it. She said it felt like a friend was telling her. Maybe we need more human touches, not just rules. Also-can we get a 'take with water' icon that doesn't look like a teapot? I thought it was for tea for weeks.
Malik Ronquillo
January 27, 2026 AT 15:20Look, I get it. People are dumb. But the real tragedy? Pharmacists know this is broken and they’re too tired to fix it. I went to CVS last week and the guy just handed me the bottle like it was a bag of chips. No explanation. No smile. No 'you good?' Just... 'next.' We’re treating medicine like a vending machine. And yeah, people mess up. But we made it easy for them to.
Brenda King
January 27, 2026 AT 23:14My mom has early dementia and I had to make a video for her with my phone showing her taking her meds. We used the same bottle, same time, same words. She watches it every morning. I wish pharmacies did this by default. A QR code that plays a 10-second video in your language? That’s not fancy-it’s basic care. We can do better.
Keith Helm
January 29, 2026 AT 12:26Legislation is required. Voluntary standards are insufficient. Mandate USP Chapter 17 compliance nationwide. Enforce penalties for non-compliance. Allocate federal funding for pharmacy software upgrades. Eliminate ambiguity. Save lives.
Daphne Mallari - Tolentino
January 29, 2026 AT 18:07It is both lamentable and emblematic of the broader degradation of public health infrastructure that pharmacological instructions continue to be rendered in a manner antithetical to the principles of patient-centered care. The persistence of archaic nomenclature, coupled with the absence of standardized visual lexicons, constitutes an unconscionable failure of institutional responsibility. One would hope for a more rigorous, evidence-based approach to pharmaceutical communication, rather than the current patchwork of goodwill initiatives and ad hoc accommodations.