Most people think generic drugs are cheap because they’re generic. But the truth? Insurers aren’t saving money just because generics exist-they’re saving because they’re bulk buying and running aggressive tendering processes that force manufacturers to compete on price. It’s not magic. It’s procurement, and it’s happening behind the scenes in every major health plan.
Why generics aren’t automatically cheap
Just because a drug is off-patent doesn’t mean it’s affordable. In 2023, the average price of a generic prescription was still $19. That sounds low-until you realize some generics cost over $1,000 a month. Why? Because when there’s only one or two manufacturers making a drug, there’s no competition. And without competition, prices stay high. The real savings come when insurers bring together hundreds of thousands of prescriptions and say: “We’ll buy 5 million pills of this generic blood pressure drug. Who can deliver it cheapest?” That’s tendering. It’s like an auction, but for medicine.How tendering works in practice
Insurers don’t just pick the cheapest bid blindly. They use formularies-lists of approved drugs-to steer patients toward the most cost-effective options. A typical formulary has tiers. Tier 1 is the cheapest. Tier 2 is a little more. Tier 3? That’s where brand names live. But here’s the twist: even within Tier 1, prices vary wildly. One manufacturer might sell amlodipine (a common blood pressure pill) for $0.15 per tablet. Another might charge $0.45. Same drug. Same FDA approval. Same effect. The insurer picks the $0.15 version and locks in a three-year contract. This isn’t theoretical. A 2022 study in JAMA Network Open found that some insurers were paying up to 90% more for certain generics simply because they didn’t know which versions were cheaper. Once they started auditing their formularies quarterly, they cut spending by 30% in six months.The middlemen problem
Most insurers don’t buy drugs directly. They use pharmacy benefit managers (PBMs)-companies like OptumRx, Caremark, and Express Scripts. These PBMs negotiate prices, manage formularies, and handle claims. Sounds helpful, right? Not always. PBMs often use a trick called “spread pricing.” They tell the insurer: “We negotiated a $10 price for this generic.” Then they tell the pharmacy: “We’ll pay you $6.” The $4 difference? That’s their profit. And here’s the kicker: they don’t have to tell the insurer. The insurer thinks they’re saving money. But the real savings are being siphoned off. That’s why some employers and health plans are cutting out the middleman. Costco, for example, sells 90-day supplies of common generics for under $10-no insurance needed. Mark Cuban’s Cost Plus Drug Company charges 15% over wholesale cost, plus a $3 fee. No spreads. No secrets. And customers save an average of 76% compared to retail pharmacies.
When cheap goes too far
There’s a dark side to aggressive tendering. When insurers demand prices so low that manufacturers can’t cover production costs, they quit. And when that happens, shortages follow. In 2020, albuterol inhalers-the lifesaving asthma medication-vanished from shelves across the U.S. Why? Because the price had been bid down to $10 per inhaler. The cost to make one? $12. So manufacturers stopped making them. Eighty-seven percent of hospitals reported shortages. It’s a classic case of “too much competition.” The system rewards the lowest bid, but doesn’t account for sustainability. The FDA now tracks this risk more closely, but there’s still no safety net for essential generics.What’s changing in 2026
The Inflation Reduction Act of 2022 was supposed to fix this. It capped insulin at $35 a month for Medicare patients. But it left PBMs untouched. Their spread pricing? Still legal. Their formulary steering? Still opaque. That’s why states like California passed laws like SB 17 in 2017, forcing PBMs to disclose any price differences over 5%. Now, insurers can see exactly how much the PBM is pocketing. Meanwhile, the FDA is speeding up generic approvals. In 2023, they approved over 1,000 new generics. The first generic for a drug usually saves $500 million to $1 billion in its first year. That’s why insurers are pushing for early access to new generics-before prices settle.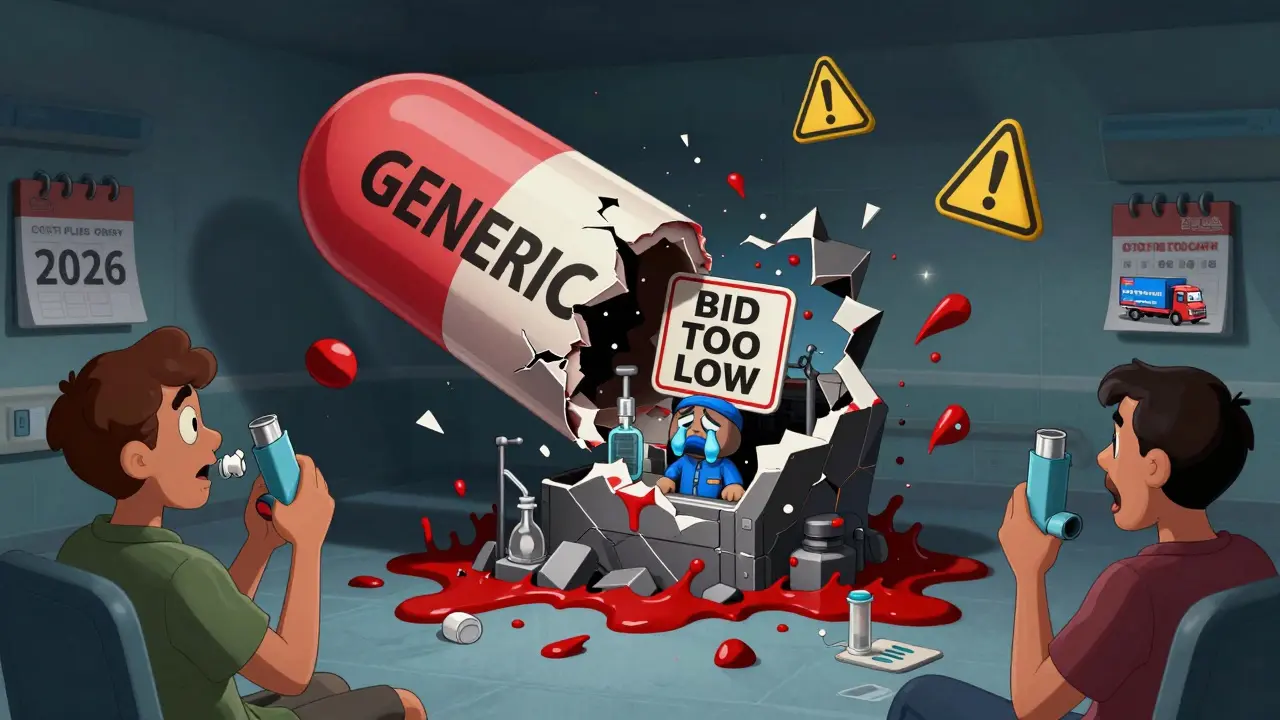
What you can do
If you’re on insurance, you might be overpaying for generics without knowing it. Here’s what to check:- Use GoodRx or SingleCare to compare cash prices vs. your insurance copay. You’ll be surprised how often cash is cheaper-even with insurance.
- Ask your pharmacist: “Is there a lower-cost version of this generic?” Sometimes the same drug is made by three different companies. One might cost $3 instead of $30.
- Check if your employer offers a direct-to-consumer pharmacy benefit. Companies like Blueberry Pharmacy and Cost Plus Drug Company are now partnering with employers to bypass PBMs entirely.
The real savings
In 2023, generic drugs saved the U.S. healthcare system $445 billion. That’s more than the entire annual budget of the Department of Education. And $194 billion of that came from adults aged 40 to 64-people who are paying for their own prescriptions. The lesson? Generics aren’t cheap because they’re generic. They’re cheap because someone fought for it. Insurers didn’t get these savings by accident. They used data, contracts, and competition. And if you know how to ask for it, you can too.Why does my insurance still make me pay $50 for a generic drug?
Your insurance may be using a PBM that practices spread pricing-meaning they charge your plan more than they pay the pharmacy, and keep the difference. The copay you see isn’t necessarily the real cost of the drug. Sometimes, paying cash with a coupon like GoodRx is cheaper than using your insurance. Always check both prices.
Can I ask my insurer to switch to a cheaper generic version?
Yes. Call your insurer’s pharmacy services line and ask: “Is there a therapeutically equivalent generic with a lower cost?” If your current generic has fewer manufacturers, it’s likely more expensive. Insurers often have lists of preferred generics and can switch you without a new prescription.
What’s the difference between a PBM and an insurer?
Your insurer (like UnitedHealth or Blue Cross) pays for your care. A PBM (like OptumRx or CVS Caremark) manages your drug benefits-they negotiate prices, create formularies, and process claims. Many PBMs are owned by insurers, which creates a conflict of interest. They profit from higher drug prices, not lower ones.
Why do some generics cost more than brand-name drugs?
Rarely, but it happens. This usually occurs when a generic drug has very few manufacturers-sometimes just one. Without competition, the manufacturer can charge more. Some older generics, like certain antibiotics or thyroid meds, fall into this category. Always compare prices with cash options.
Is it safe to buy generics from direct-to-consumer pharmacies?
Yes-if they’re FDA-approved. Companies like Cost Plus Drug Company and Blueberry Pharmacy source from licensed U.S. distributors and list their wholesale costs transparently. Their drugs are the same as those in your local pharmacy-just priced 70-90% lower because they cut out middlemen. Always check if the pharmacy is verified by the National Association of Boards of Pharmacy (NABP).


Paul Mason
January 6, 2026 AT 18:43Man, I never realized how much of a scam PBMs are. I thought my insurance was saving me money, but turns out they’re just letting some middleman pocket the difference. I started using GoodRx last year and now I pay $4 for my blood pressure med instead of $45. Why does anyone still use insurance for generics? It’s like paying a toll to walk down your own street.
Also, Costco’s generics are insane. I bought a 90-day supply of metformin for $7. No joke. My pharmacist said the same pill costs $38 at my local pharmacy with insurance. Someone’s making bank and it ain’t me.
Mina Murray
January 7, 2026 AT 22:35Yeah right. And I’m sure the FDA is just sitting around waiting for you to tell them what to do. You think this is about savings? Nah. It’s about control. The government lets PBMs run wild so they can blame ‘big pharma’ when prices go up. Meanwhile, your insulin’s capped at $35 but your blood pressure med still costs $50 because the system’s rigged to keep you dependent. Wake up.
They’re not trying to save you. They’re trying to make you think you’re saved.
Elen Pihlap
January 9, 2026 AT 02:44I’ve been paying $60 for my asthma inhaler for years. I just found out the generic costs $8 cash. I feel so stupid. Like, why did I trust my insurance? Why did I never ask? I’m mad at myself more than anyone else. I just kept thinking ‘it’s insurance, it’s supposed to help.’ Turns out it’s just another bill.
Christine Joy Chicano
January 9, 2026 AT 20:45What’s wild is how the same exact molecule, same FDA approval, same clinical effect, can cost 300% more just because of who made it. It’s like buying a Honda Civic and paying $40k because the dealership says ‘this one’s special.’
Generics aren’t cheap because they’re generic. They’re cheap because someone finally stopped treating them like they’re invisible. The system treats patients like data points and drugs like commodities. But pills don’t care about spreads or formularies. They just want to work.
Anastasia Novak
January 10, 2026 AT 13:20Oh my god. I just looked up my levothyroxine. I’ve been paying $42 with insurance. Cash price? $12. I cried. Not because I’m emotional, but because I’ve been robbed for 7 years. And my PBM? They’re owned by my insurer. So they profit from my suffering. This isn’t healthcare. It’s a pyramid scheme with stethoscopes.
Emma Addison Thomas
January 11, 2026 AT 00:42I live in the UK and we get generics for pennies through the NHS. It’s not perfect, but at least we don’t have to play detective to find out what our medicine really costs. I wish more people knew how simple this could be. Competition isn’t the problem-it’s the layers of middlemen hiding behind ‘efficiency.’
Rachel Steward
January 11, 2026 AT 10:33Let’s not pretend this is about ‘savings.’ It’s about power. The entire system is engineered to keep patients confused and compliant. Insurers don’t want you to know the cash price. PBMs don’t want you to know they’re pocketing $4 per pill. Manufacturers don’t want you to know that $0.15 vs $0.45 is the same damn tablet.
This isn’t capitalism. It’s rent-seeking dressed up as healthcare. And the worst part? We’re all complicit because we’re too tired to fight it. So we pay. And pay. And pay.
Meanwhile, the people who actually make the drugs? They’re getting squeezed out. The system rewards greed, not health.
Sai Ganesh
January 11, 2026 AT 16:54In India, we have a similar issue but with a twist. Many generics are produced locally at very low cost, but quality control is inconsistent. So while price is low, safety isn’t guaranteed. The US system has its flaws, but at least the FDA ensures consistency. Maybe the real solution isn’t cutting out middlemen, but regulating them better.
Transparency is key. If PBMs had to disclose every spread, and insurers had to publish their formulary pricing publicly, we’d see real change. Not just for Americans-for global patients too.
Katrina Morris
January 12, 2026 AT 23:09my pharmacist just told me there’s a cheaper version of my antidepressant and i didn’t even know it existed. i feel like a idiot for never asking. i’m gonna start checking cash prices every time. also i just found out cost plus drug co ships to my state?? wow. thank you for this post. i’m gonna share it with my mom.
Kyle King
January 13, 2026 AT 07:07Big Pharma + PBMs + Insurance = The Great Drug Heist. It’s all a lie. The government knows. The FDA knows. They’re letting this happen so they can sell you ‘affordable’ insulin while your other meds cost a mortgage. And now they’re pushing ‘generic competition’ like it’s a fix. It’s not. It’s a distraction. They want you to think it’s about price… when it’s really about control. Wake up. The pills are fine. The system is the poison.
Jonathan Larson
January 15, 2026 AT 01:02It is worth noting that the structural inefficiencies described herein are not unique to pharmaceuticals-they are systemic features of complex, fragmented markets where information asymmetry is weaponized. The solution lies not in vilifying any single actor, but in institutional redesign: mandatory price transparency, elimination of spread pricing, and incentivizing value-based formularies over cost-based ones.
Patients are not consumers in the traditional sense. They are vulnerable actors in a high-stakes, emotionally charged domain. Policies must reflect that reality, not market dogma. The $445 billion saved in 2023 is admirable, but it should not come at the cost of access, safety, or dignity.
Let us not mistake efficiency for ethics.