QT Interval Calculator
The QT interval is a key measurement on an ECG that shows the time it takes for your heart's electrical system to recharge between beats. Some medications can lengthen this interval, increasing the risk of dangerous heart rhythms like torsades de pointes.
Feeling your heart race for no obvious reason? Maybe you just climbed the stairs, had too much coffee, or were stressed. But what if you didn’t? What if your heart started pounding after you started a new pill - something your doctor prescribed, or even something you bought over the counter? You’re not alone. Medications are one of the most common, yet often overlooked, causes of palpitations and rapid heartbeat. And while many cases are harmless, some can be serious - even life-threatening.
What Exactly Are Medication-Induced Palpitations?
Palpitations are when you feel your heart beating too hard, too fast, or irregularly. It’s not just a quick flutter. It can feel like your chest is thumping, your throat is tight, or you’re about to pass out. When these symptoms show up after starting a new medication, it’s not coincidence - it’s a known side effect. Over 150 prescription and over-the-counter drugs can trigger this. Some do it by speeding up your heart directly. Others mess with your heart’s electrical signals, leading to dangerous rhythms like torsades de pointes, a type of rapid, chaotic heartbeat that can turn fatal if not treated.
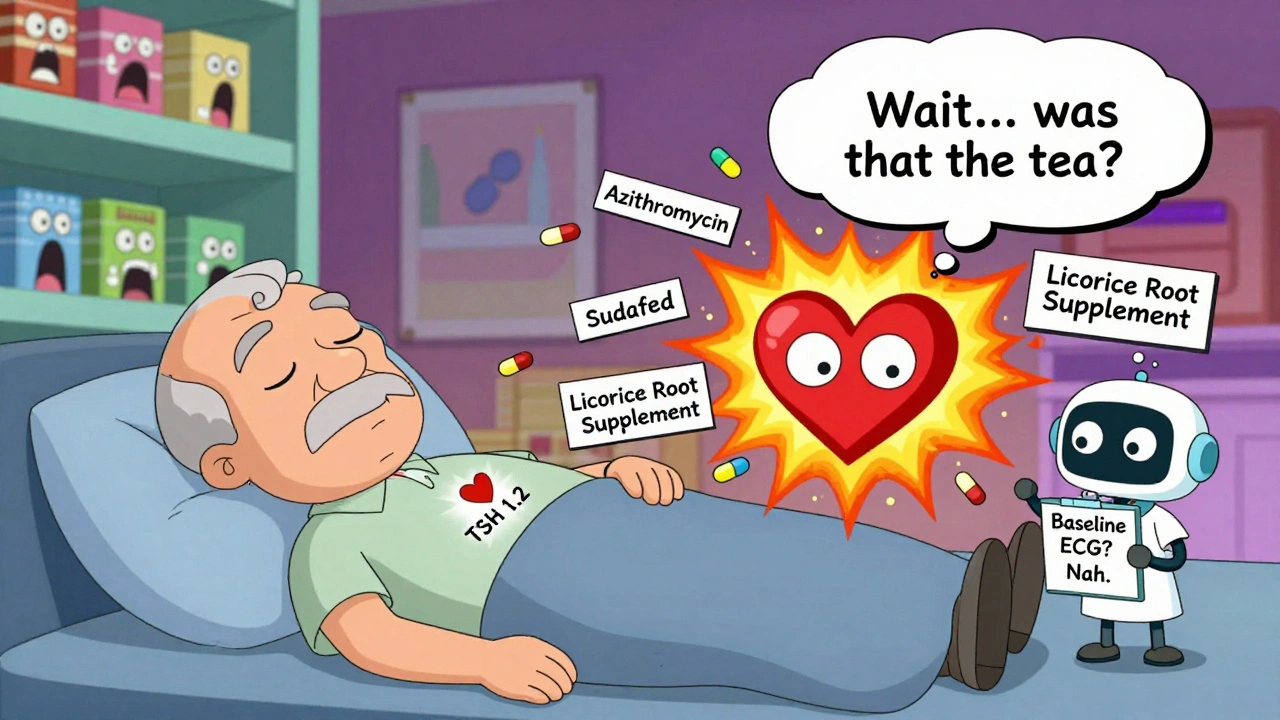
The American Heart Association says medication-related arrhythmias make up 10-20% of all cases seen in clinics. In older adults or people with existing heart conditions, that number jumps even higher. The key? It’s not always the drug itself. It’s the combo - taking two medications that both stretch your heart’s electrical timing, or having low potassium or magnesium while on a risky pill. That’s when things go from annoying to dangerous.
Top Medications That Trigger Rapid Heartbeat
Not all drugs are created equal when it comes to heart risks. Some are well-known culprits. Others sneak in under the radar.
- Asthma inhalers like albuterol (salbutamol) are common. They’re lifesavers for breathing, but they can jack up your heart rate by 15-25 beats per minute within half an hour. That’s normal for some - but if you’re already prone to arrhythmias, it’s a red flag.
- Antibiotics like azithromycin (Zithromax) are among the biggest offenders. A 2021 study of 1.2 million people found azithromycin more than doubles the risk of dangerous rapid heart rhythms. Levofloxacin and ciprofloxacin also carry risks, though lower. If you’ve got heart disease or an old ECG showing a long QT interval, ask your doctor about amoxicillin instead.
- Decongestants like pseudoephedrine (Sudafed) are everywhere. At 60mg, they can raise your heart rate by 10-20 bpm. Phenylephrine is similar but weaker. If you’re over 60 or have high blood pressure, skip these. Use saline sprays or humidifiers instead.
- Thyroid meds like levothyroxine (Synthroid) are often blamed for palpitations. But it’s rarely the drug itself - it’s the dose. When your TSH drops below 0.1 mIU/L, you’re likely getting too much. That triggers a racing heart, sweating, and anxiety. Most cases fix themselves with a small dose reduction and retesting TSH in 4-6 weeks.
- Antidepressants vary. Amitriptyline (a tricyclic) can stretch your QT interval by 40-60ms - dangerous territory. Citalopram (Celexa) is the worst offender among SSRIs, especially above 40mg/day. Sertraline (Zoloft) and escitalopram (Lexapro) are much safer for the heart. If you’re on citalopram and feel your heart pounding, talk to your doctor about switching.
- Newer weight-loss drugs like semaglutide (Ozempic, Wegovy) are surprising players. Clinical trials show they raise heart rate by 3-5 bpm on average. For most, that’s fine. But if you already have heart disease or palpitations, it’s worth monitoring.
How Doctors Evaluate Medication-Induced Palpitations
If you’re experiencing palpitations and you’re on any medication, your doctor needs to treat this like a medical puzzle - not just a symptom to ignore. Here’s what they should check:
- Full medication list - every pill, patch, supplement, and herbal product. Even “harmless” ones like St. John’s Wort or licorice root can interfere.
- ECG (electrocardiogram) - this is non-negotiable. It measures your heart’s electrical rhythm and calculates your QTc interval. Normal is under 450ms for men, 460ms for women. Above 500ms? High risk. An increase of more than 60ms from your baseline? Also high risk.
- Electrolytes - low potassium (<3.5 mmol/L) or low magnesium (<1.7 mg/dL) make your heart way more sensitive to bad drug effects. These are easy to fix with supplements or diet.
- Thyroid test (TSH) - if you’re on levothyroxine, this tells you if your dose is too high.
- 24-48 hour Holter monitor - if your resting ECG looks normal but you still feel your heart racing, this portable device records your heart’s activity while you go about your day. It catches intermittent problems 35-45% of the time.
Some hospitals use a risk-scoring tool that adds points for age (over 65 = +2), female sex (+1), and each additional QT-prolonging drug (+3). A score above 5 means you’re at high risk and need urgent action.

What to Do If Medications Are Causing Your Palpitations
Don’t panic. Don’t stop cold turkey. But do act.
Mild cases - no symptoms, QTc under 500ms, no heart disease? Your doctor may say: keep taking it, but get a repeat ECG in a week. Fix your potassium and magnesium. Avoid caffeine and alcohol. Track your heart rate daily with a smartwatch or manual pulse check.
Moderate cases - palpitations, QTc between 480-500ms? Dose reduction often works. Studies show 60-70% of patients feel better within 72 hours of lowering the dose. For example, switching from 40mg to 20mg of citalopram can eliminate palpitations without losing antidepressant benefits.
High-risk cases - QTc over 500ms, fainting, or a documented arrhythmia? Stop the drug immediately. This isn’t optional. Hospitals follow strict protocols: discontinue the culprit, monitor in the ER, and correct electrolytes. In severe cases, doctors may give magnesium sulfate intravenously to stabilize the heart rhythm.
And when you need to replace the drug? Options exist. For antibiotics, amoxicillin is safer than azithromycin. For depression, sertraline beats citalopram. For thyroid issues, slow titration keeps TSH between 0.5 and 2.0 mIU/L - cutting palpitation risk from 12% to under 5%.
Prevention Is the Best Medicine
The best way to avoid medication-induced palpitations? Stop them before they start.
As of 2024, 92% of U.S. academic hospitals follow a new protocol: before starting high-risk drugs, they require:
- A baseline ECG within 30 days
- Electrolyte levels checked within 7 days
- Patient education on symptoms to watch for
- A follow-up ECG within 7 days if your QTc was already over 430ms
Electronic health records now auto-alert doctors if a patient has a long QTc or is being prescribed two risky drugs together. Epic Systems’ QTc Alert Module blocks dangerous prescriptions in 67% of U.S. hospitals - preventing an estimated 8,500 risky orders every month.
For older adults - especially over 75 - the risk of torsades de pointes is over three times higher. The American Geriatrics Society says: avoid QT-prolonging drugs unless absolutely necessary. And never combine them.
Dr. John Day, a leading heart rhythm expert, recommends keeping a simple medication symptom journal. Write down:
- What you took
- When you took it
- What time you felt palpitations
- Your heart rate (if you checked it)
Within days, patterns emerge. You’ll know if your heart races 30 minutes after your inhaler, or 2 days after your antibiotic. That’s power. That’s control.
Red Flags You Should Never Ignore
Some situations are clear emergencies. These are called “never events” by the Heart Rhythm Society - things that should never happen if care is done right:
- Putting two QT-prolonging drugs together - risk jumps 5.7 times
- Giving high-dose ondansetron (for nausea) to someone with QTc over 450ms
- Using fluoroquinolones in someone with heart failure - increases death risk by 18%
- Prescribing more than 40mg/day of citalopram to someone over 60
- Starting levothyroxine without an ECG in someone with known heart disease
If you’ve been told any of these are okay, get a second opinion.
Real Stories, Real Lessons
On Reddit, one user described starting azithromycin for a sinus infection. Two days later, her heart started pounding so hard she could feel it in her throat. She went to the ER. Her QTc was 540ms. They stopped the antibiotic, gave her magnesium, and she was fine in 24 hours. She now keeps a list of all her meds and checks her heart rate before taking anything new.
Another, on a thyroid medication, woke up every morning with her heart racing. Her doctor lowered her dose. Within two weeks, it was gone. Her TSH went from 0.05 to 1.2.
And a cancer patient on trastuzumab noticed palpitations only during infusions - not at other times. Her oncologist added metoprolol. The palpitations stopped. Her treatment continued safely.
These aren’t rare. They’re predictable. And they’re preventable.
Can over-the-counter meds cause rapid heartbeat?
Yes. Common OTC drugs like pseudoephedrine (Sudafed), phenylephrine, and even some weight-loss supplements or energy boosters can raise heart rate. Antihistamines like diphenhydramine (Benadryl) can also prolong the QT interval. Always read labels and talk to your pharmacist before taking anything new - especially if you have heart issues or take other medications.
How do I know if my palpitations are from medication or anxiety?
Anxiety-related palpitations often come with sweating, trembling, or a sense of dread. Medication-induced ones usually start shortly after taking the drug and feel more rhythmic - like your heart is skipping or pounding in a pattern. The key is timing. If your palpitations began 1-3 days after starting a new pill, it’s likely drug-related. A simple journal tracking meds and symptoms will show the link. An ECG can confirm if there’s a dangerous electrical change.
Is it safe to stop a medication if I feel palpitations?
Don’t stop abruptly unless you’re having chest pain, fainting, or severe dizziness. Some drugs - like beta-blockers or thyroid meds - need to be tapered. But if your QTc is over 500ms or you’re diagnosed with torsades de pointes, stopping the drug is urgent. Always contact your doctor first. They can guide you on safe discontinuation or safe alternatives.
Can supplements cause palpitations?
Absolutely. Licorice root can lower potassium. Green tea extract in high doses can stimulate the heart. Some weight-loss supplements contain hidden stimulants like synephrine or caffeine analogs. Even high-dose vitamin D or calcium can interfere with heart rhythm if you’re on certain heart meds. Always tell your doctor about every supplement you take - even if you think it’s "natural."
Should I get an ECG before starting a new medication?
If you’re over 60, have heart disease, high blood pressure, or are taking any drug known to affect heart rhythm - yes. Even if you feel fine. A baseline ECG takes 10 minutes and can prevent a hospital visit later. Many hospitals now require it for high-risk drugs like azithromycin, fluoroquinolones, and certain antidepressants. Ask your doctor: "Is this medication on the QT-prolonging list? Should I get an ECG first?"
What’s Next?
The future is getting smarter. Researchers are now testing genetic tests to find people who metabolize drugs slowly - making them far more likely to have dangerous side effects. If you’re a CYP2D6 poor metabolizer, even normal doses of certain meds can be risky. This isn’t science fiction - it’s coming to clinics soon.
For now, your best tools are awareness and communication. Know your meds. Know your numbers. Know your body. Keep a symptom log. Ask questions. Don’t assume a pill is safe just because your doctor prescribed it. If your heart feels off after a new drug, speak up. You might just save your own life.




olive ashley
December 5, 2025 AT 13:21They don't tell you this, but Big Pharma *wants* you to feel your heart race. It means more pills. More visits. More profit. They hide the QT prolongation risks in tiny print while marketing 'miracle' drugs. I've seen it with my own eyes - my mom died after they put her on citalopram. They called it 'natural aging.' It wasn't.
Dan Cole
December 6, 2025 AT 11:14Let me be perfectly clear: the notion that over-the-counter decongestants are 'harmless' is a catastrophic oversimplification. The pharmacokinetic interaction between pseudoephedrine and beta-adrenergic receptors is not merely 'a side effect'-it is a clinically significant adrenergic cascade that can precipitate ventricular tachycardia in susceptible individuals. The AHA data you cite? Underpowered. The real crisis is systemic iatrogenesis.
Billy Schimmel
December 7, 2025 AT 18:29Man, I thought I was just anxious. Turns out my Sudafed habit was making my heart do the cha-cha. Switched to saline spray. No more panic attacks at the grocery store. Sometimes the fix is dumb simple. Who knew?
Inna Borovik
December 9, 2025 AT 17:08Oh please. You list levothyroxine as a culprit? That's like blaming the thermometer for the fever. If your TSH is below 0.1, you're overdosed-not because the drug is bad, but because your doctor is lazy. I've had 12 patients in the last year whose palpitations vanished after a 12.5mcg reduction. It's not the medication. It's the incompetence.
Rashmi Gupta
December 11, 2025 AT 04:06Western medicine is broken. In India, we treat palpitations with ashwagandha, pranayama, and time. Not more pills. You Americans turn every heartbeat into a crisis needing a prescription. This article is just another way to sell fear.
Andrew Frazier
December 12, 2025 AT 10:58Who the hell is this doctor? Probably some Ivy League elitist who thinks we’re all dumb. Azithromycin? That’s a lifesaver for real people. You want us to switch to amoxicillin? That’s what the rich people take. We got jobs, we can’t wait 3 days for antibiotics to kick in. Your 'risk' is just your privilege talking.
Mayur Panchamia
December 12, 2025 AT 12:56HALT! STOP! LISTEN! The truth is buried under layers of corporate lies! Semaglutide? It’s not just raising heart rate-it’s rewiring your autonomic nervous system! They’re testing it on the poor, the elderly, the vulnerable! You think this is about weight loss? NO! It’s about population control! Look at the patents! Look at the funding! The WHO is in on it!!
Karen Mitchell
December 13, 2025 AT 14:54This article is dangerously irresponsible. It provides no citations for the 150-drug claim. It misrepresents the QT interval thresholds. It fails to differentiate between transient sinus tachycardia and true arrhythmias. And it encourages patients to self-diagnose based on anecdotal symptoms. This is not medical advice. This is fearmongering dressed as public health.
Nava Jothy
December 15, 2025 AT 07:21I’ve been on Lexapro for 7 years. My heart never raced until I started drinking green tea with lemon. 😔 Now I cry every time I take my pill. My therapist says it’s 'emotional dysregulation.' But I know. It’s the pills. The system. The silence. 🥺💔
brenda olvera
December 16, 2025 AT 20:16My grandma in Texas took azithromycin for a cold and lived to 98. She danced at her own wedding. Maybe your body knows what to do. Don’t fear the medicine. Fear the fear itself. 🌞
Ibrahim Yakubu
December 16, 2025 AT 22:01In Nigeria, we don't have access to ECGs. We don't have doctors who know QT intervals. We have pharmacies with no training. If you feel your heart racing, you buy ginger and pray. This article? It's for people who can afford to worry. We just survive.
Chris Park
December 17, 2025 AT 07:50They’re hiding the truth again. The FDA knows. The CDC knows. But they won’t say it: all these drugs are designed to create chronic conditions. Palpitations? That’s not a side effect-that’s a feature. It keeps you coming back. They profit from your fear. Your anxiety. Your heartbeat. Wake up.
Priya Ranjan
December 18, 2025 AT 03:29It’s not the drugs. It’s the lack of spiritual discipline. People take pills like candy and then blame the medication. If you meditated, fasted, and lived in alignment with nature, you wouldn’t need half of these. But no-you want quick fixes. You want convenience. And now you’re surprised your heart is out of sync? Pathetic.
Gwyneth Agnes
December 18, 2025 AT 20:44Stop taking so many pills.
olive ashley
December 20, 2025 AT 18:38Exactly. And then they add another pill for the side effect. Then another for that. It’s a pyramid scheme. I saw a guy on Reddit who was on 17 meds. His heart was a drum. He didn’t even know which one was the problem. They call it polypharmacy. I call it medical abuse.