Some medications are like walking a tightrope. One step too far, and things can go wrong-fast. These are called narrow therapeutic index drugs, or NTI drugs. They work well when taken exactly as prescribed. But even a small change in dose-or switching brands-can push you from safe to dangerous, or from effective to useless. If you’re taking one of these drugs, you need to know how they work, why they’re different, and what you can do to stay safe.
What Makes a Drug Have a Narrow Therapeutic Index?
Every drug has a sweet spot: the amount in your blood that treats your condition without causing harm. For most medicines, there’s a wide buffer-like driving with plenty of space between you and the car ahead. But for NTI drugs, that buffer is razor-thin. The difference between the lowest dose that works and the lowest dose that causes harm is often less than double. That means if your blood level goes up just 10-20%, you could hit toxic levels. Drop it by the same amount, and the drug stops working.
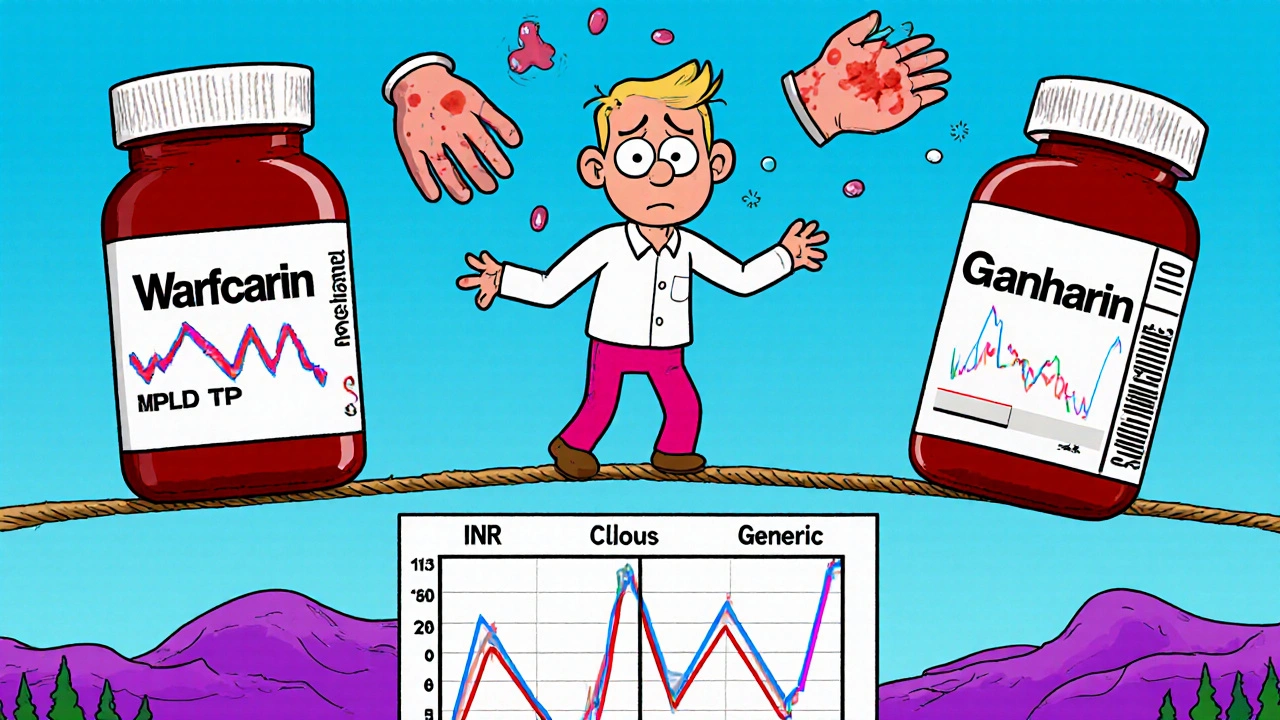
Take warfarin, for example. It prevents blood clots. The target level is measured by something called INR. A reading between 2.0 and 3.0 is ideal. Go above 3.5, and you risk dangerous bleeding-even from a minor bump. Drop below 2.0, and you could get a stroke or clot in your leg. One study found that switching generic brands caused INR levels to spike in 1 in 5 patients, leading to emergency treatment.
Lithium, used for bipolar disorder, is another example. The safe range is 0.6 to 1.2 mmol/L. Go above 1.5, and you might start shaking, feeling confused, or even have seizures. Below 0.6, your mood swings can return. There’s almost no room for error.
Common NTI Drugs You Might Be Taking
You might not realize you’re on an NTI drug. Here are the most common ones:
- Warfarin (Coumadin, Jantoven) - Blood thinner
- Lithium (Lithobid) - Mood stabilizer
- Levothyroxine (Synthroid, Tirosint) - Thyroid hormone replacement
- Digoxin (Lanoxin) - Heart medication
- Tacrolimus (Prograf) - Immunosuppressant after organ transplant
- Phenytoin (Dilantin) - Seizure control
- Carbamazepine (Tegretol) - Seizure and nerve pain treatment
- Methotrexate (Trexall) - Used for autoimmune diseases and some cancers
Each of these has a tiny window where it works. Digoxin’s safe range is 0.5 to 0.9 ng/mL. Above 2.0, it can cause deadly heart rhythms. Tacrolimus levels must stay between 5 and 15 ng/mL after a transplant-too low, and your body rejects the new organ; too high, and your kidneys get damaged.
Why Generic Switches Can Be Risky
Generic drugs are usually safe and save money. But with NTI drugs, even tiny differences in how the body absorbs the medicine can matter. A generic version might look identical, but the way it dissolves or is absorbed can vary slightly. For most drugs, that’s fine. For NTI drugs, it’s not.
The U.S. Food and Drug Administration (FDA) requires standard generics to be within 80-125% of the brand-name drug’s absorption. But for NTI drugs, that’s too wide. Experts and regulators now agree that for these medications, the range should be much tighter-90-111%. Some states, like North Carolina, now require pharmacists to get your doctor’s approval before switching your NTI drug to a generic.
Patients report real problems. One warfarin user switched from brand-name Coumadin to a generic and saw their INR jump from 2.5 to 4.1 in just one week. That’s a bleeding risk. Another person switching levothyroxine brands saw their TSH level go from 1.8 to 8.4 in six weeks-causing extreme fatigue and weight gain. These aren’t rare cases. In one survey, 63% of NTI drug users needed a dose change within three months of starting therapy, and over 30% had a serious event tied to blood level changes.
Monitoring Is Not Optional-It’s Lifesaving
If you’re on an NTI drug, regular blood tests aren’t a suggestion. They’re essential. Here’s what’s typically needed:
- Warfarin: INR test every 1-4 weeks, especially when starting or changing doses
- Lithium: Blood level check every 3-6 months, more often when adjusting dose
- Levothyroxine: TSH test every 6-8 weeks after a dose change, then every 6-12 months if stable
- Digoxin: Blood level every 6-12 months, or if symptoms appear
- Tacrolimus: Twice weekly at first after transplant, then weekly or monthly as you stabilize
Skipping these tests is like driving blindfolded. You won’t know you’re in danger until it’s too late. Patients who track their levels, symptoms, and medication changes using a simple journal or app have 32% fewer bad outcomes than those who don’t.
What to Watch For: Signs of Too Much or Too Little
You need to know the early warning signs. Don’t wait for a crisis.
For warfarin:
- Too much: Unexplained bruising, nosebleeds, blood in urine or stool, headaches, dizziness
- Too little: Swelling or pain in legs, chest pain, shortness of breath, sudden weakness
For lithium:
- Too much: Hand tremors, nausea, confusion, slurred speech, muscle weakness, blurred vision
- Too little: Return of mood swings, irritability, depression, lack of energy
For levothyroxine:
- Too much: Rapid heartbeat, sweating, weight loss, anxiety, insomnia
- Too little: Fatigue, weight gain, cold intolerance, dry skin, depression
If you notice any of these, call your doctor. Don’t wait. Your next blood test might be too late.
How to Stay Safe Every Day
Here’s what you can do right now to protect yourself:
- Stick to one brand or generic. If your pharmacy switches your drug, ask if it’s the same one you’ve been taking. Don’t accept a change without checking with your doctor.
- Take it at the same time every day. Especially for levothyroxine and warfarin, timing matters. Take levothyroxine on an empty stomach, at least 30-60 minutes before food.
- Watch what you eat and drink. Vitamin K (in leafy greens) affects warfarin. Grapefruit can interfere with tacrolimus and carbamazepine. Alcohol can raise lithium levels.
- Keep a simple log. Write down your dose, any symptoms, and when you had your blood test. Bring it to every appointment.
- Ask about pharmacogenetic testing. New research shows your genes can tell doctors how your body processes drugs like warfarin and phenytoin. This can help find your right dose faster.
What’s Changing in NTI Drug Care
The system is catching up. The FDA is working on a formal list of NTI drugs with clear rules for testing. By 2024, they plan to finalize which drugs need tighter standards for generics. Hospitals are now using barcode scans for high-risk NTI drugs to prevent dosing errors. And three FDA-approved apps are now available to help patients track doses, symptoms, and lab results.
Researchers are also studying how genetics affect drug response. Early results show that for warfarin, two genes (CYP2C9 and VKORC1) explain up to 60% of why people need different doses. By 2026, genetic testing before starting these drugs may become standard. That could cut adverse events by a third.
NTI drugs aren’t going away. But with better tools, better rules, and better patient awareness, they’re becoming safer to use.
Frequently Asked Questions
Are all generic drugs unsafe for NTI medications?
No. Many generic versions of NTI drugs are safe and work just as well as brand names. But not all generics are created equal. Some have slight differences in how they’re made that can affect absorption. That’s why it’s important to stick with the same manufacturer unless your doctor approves a switch. Always check the label for the manufacturer’s name and ask your pharmacist if the generic you’re getting is the same one you’ve used before.
Can I stop taking my NTI drug if I feel fine?
Never stop or change your dose without talking to your doctor. Even if you feel fine, your blood level might be too low or too high. Many people on NTI drugs feel normal until something goes wrong-like a clot, seizure, or organ rejection. Your symptoms don’t always match your blood levels. That’s why regular testing is critical.
How often do I really need blood tests?
It depends on the drug and how stable you are. When you first start, you’ll need frequent tests-weekly or biweekly. Once your levels are steady, you might only need them every few months. But if you get sick, start a new medicine, change your diet, or switch pharmacies, you’ll need a test sooner. Your doctor will tell you the schedule, but always call if you feel off-even if your next test isn’t due yet.
What should I do if I miss a dose?
Don’t double up. For most NTI drugs, missing one dose won’t cause immediate harm, but it can throw off your balance over time. Call your doctor or pharmacist for advice. For levothyroxine, take it as soon as you remember, unless it’s close to your next dose. For warfarin, skip the missed dose and go back to your regular schedule. Never guess-always check.
Can I use over-the-counter medicines or supplements with NTI drugs?
Many OTC products can interfere. Ibuprofen and aspirin can increase bleeding risk with warfarin. St. John’s wort can lower levels of tacrolimus and carbamazepine. Calcium and iron supplements can block levothyroxine absorption. Always tell your doctor and pharmacist about everything you take-even vitamins, herbs, or teas. What seems harmless might be dangerous with your NTI drug.
Next Steps for Patients
If you’re on an NTI drug, here’s what to do today:
- Check your last blood test result. Do you know what it was?
- Look at your prescription bottle. Is it the same brand or generic as last month?
- Write down any symptoms you’ve noticed in the past month-even small ones.
- Call your doctor’s office and ask: “Is my drug on the NTI list? Do I need more frequent testing?”
- Download a free medication tracker app (like Medisafe or MyTherapy) to log doses and symptoms.
NTI drugs aren’t dangerous if you understand them. They’re powerful tools. But they demand attention. With the right knowledge and habits, you can take them safely-and live well.


Andrew Forthmuller
November 14, 2025 AT 06:47My INR jumped to 4.8 after a generic switch. ER visit. Never again.
Renee Ruth
November 15, 2025 AT 04:13They say generics are ‘bioequivalent’ but that’s corporate nonsense. I’ve seen people crash on lithium switches-hospitalized, confused, shaking. The FDA’s 80-125% rule is a death sentence for NTI drugs. No wonder so many of us end up in psych wards or ICU. This isn’t about savings. It’s about control. And they don’t care.
My cousin died from a tacrolimus switch after her transplant. They told her it was ‘the same.’ Same? The lab results looked like a rollercoaster. They didn’t even retest for two weeks. Two weeks. She had a seizure on a Tuesday. By Friday, her kidneys were failing. No one took responsibility.
I keep a spreadsheet. Every dose. Every lab. Every pharmacy change. I’ve got 17 months of data. Every single time they switched my levothyroxine, my TSH went haywire. I had to beg for my original brand. My doctor rolled his eyes. Said ‘it’s just a pill.’
They don’t get it. This isn’t ibuprofen. You can’t just ‘take it and see.’ One milligram too much and your brain starts glitching. One milligram too little and your heart skips. It’s not a drug. It’s a minefield.
And now they want to push genetic testing like it’s magic? Cool. But what about the people who can’t afford it? Or live in states where pharmacists don’t even have to ask? You think your ‘safe’ generic is safe until you’re the one bleeding out on the bathroom floor.
Don’t trust the system. Trust your body. And if you feel off? Don’t wait for your next test. Call your doctor. Now.
Samantha Wade
November 15, 2025 AT 05:37While the anecdotal evidence presented is compelling, it is imperative to recognize that the FDA’s bioequivalence standards are grounded in rigorous pharmacokinetic modeling and population-level data. That said, the clinical variability observed in NTI drugs-particularly with warfarin and levothyroxine-does warrant a more nuanced regulatory approach. The proposed 90–111% absorption window is scientifically justified and aligns with guidelines from the European Medicines Agency.
Pharmacists must be empowered with clear protocols for NTI substitutions, and electronic health record integration should flag these drugs automatically. Furthermore, patient education materials should be standardized across providers to ensure consistent messaging. The data showing a 32% reduction in adverse events with patient tracking apps is not merely encouraging-it is transformative. We must scale these tools systematically, not rely on individual vigilance alone.
Genetic testing for CYP2C9 and VKORC1 variants is not a luxury; it is a clinical necessity for warfarin initiation. The cost-benefit analysis favors implementation, especially given the high cost of hospitalizations due to INR instability. We owe it to patients to move beyond ‘one-size-fits-all’ prescribing.
Elizabeth Buján
November 15, 2025 AT 19:54Okay so i was on levothyroxine for 3 years and my doc kept switching the generic and i kept getting so tired like i couldnt even get out of bed and my hair was falling out and i was crying for no reason and i thought i was just… broken? like maybe i was just lazy or depressed? but then i started keeping a journal and i noticed the pattern-every time the pill looked different, i felt worse.
so i finally told my doctor ‘i need the same brand, no matter the cost’ and she was like ‘oh honey, it’s all the same’ and i just looked at her and said ‘then why do i feel like a zombie every time you change it?’
she finally listened. switched me back. i got my energy back. my hair grew back. i stopped crying for no reason.
it’s not in my head. it’s in the pill. and if you’re on one of these drugs and you feel ‘off’-trust that. don’t let anyone tell you it’s ‘all in your head.’ your body knows. i promise.
also-st john’s wort is a trap. don’t touch it. i tried it for ‘anxiety’ and nearly went to the hospital. just say no.
vanessa k
November 16, 2025 AT 01:00I’ve been on tacrolimus since my kidney transplant five years ago. Twice a week blood draws, every single week. I don’t miss one. I don’t skip. I don’t let the pharmacy switch my brand. I’ve had two different generics. One made me shake like I had Parkinson’s. I called my transplant team immediately. They told me to stop it and go back. No questions.
I keep a little notebook in my purse. Dose. Time. Symptoms. Lab numbers. I bring it to every appointment. My nurse says I’m the most organized patient she’s ever had. I tell her: I’m not organized. I’m just scared.
People think because I’m ‘stable’ now, I’m fine. But I’m not fine. I’m just surviving. And I won’t risk it for a few bucks at the pharmacy.
Don’t let anyone tell you it’s ‘just a pill.’ It’s your life.
manish kumar
November 16, 2025 AT 22:59As someone who has been managing phenytoin for epilepsy for over a decade, I can attest that the variability in generic formulations is not just a theoretical concern-it is a daily reality. In India, where access to brand-name drugs is often limited due to cost, the burden falls disproportionately on patients who must navigate inconsistent generics with minimal monitoring infrastructure. I have personally witnessed seizures triggered by unannounced generic switches in rural clinics where blood level testing is either unavailable or prohibitively expensive.
While the U.S. has made strides in recognizing NTI drug risks, many low- and middle-income countries lack even the most basic pharmacovigilance systems. The FDA’s proposed tightening of bioequivalence standards to 90–111% is commendable, but without global harmonization, patients elsewhere remain vulnerable. International pharmaceutical regulators must collaborate to establish universal NTI drug guidelines, including mandatory patient registries and real-time adverse event reporting.
Additionally, community health workers should be trained to recognize early signs of toxicity or underdosing, especially in areas where neurologists are scarce. Simple symptom checklists distributed at pharmacies could save lives. Education must extend beyond the clinic walls.
Finally, I urge pharmaceutical manufacturers to prioritize batch consistency over profit margins. A patient’s life should not hinge on which factory produced their medication. We need transparency in sourcing, labeling, and quality control-not just for NTI drugs, but for all critical medications worldwide.
Nicole M
November 18, 2025 AT 16:18Wait so if I switch from Synthroid to a generic and my TSH goes from 2.1 to 7.9, that’s not normal? I thought all thyroid meds were the same. My doctor said ‘it’s just the pill’ and I believed her. Then I got so tired I missed work for two weeks. I had to beg to get my original brand back. Now I’m paranoid every time I fill my script. I even take a pic of the pill before I leave the pharmacy.
Also-why does no one talk about how hard it is to get blood tests? My insurance only covers them every 6 months, but I need them every 2. I’m lucky I have PTO to go. What about people who work two jobs?
This whole system feels like a trap.
Arpita Shukla
November 20, 2025 AT 04:37You all are overreacting. The FDA doesn’t approve bad generics. If your levels are off, it’s probably because you’re not taking it right. Maybe you’re eating with your levothyroxine. Maybe you’re drinking grapefruit juice with your tacrolimus. Or maybe you’re just bad at following instructions.
My cousin takes lithium and she’s fine. She switches generics all the time. No issues. You’re making this into a drama. It’s just medicine. Take it like an adult.
Also, genetic testing? That’s for rich people. Most of us can’t afford it. Just take the pill they give you and stop complaining.
And no, St. John’s Wort doesn’t ‘nearly kill you.’ That’s just internet fearmongering. I’ve taken it for years with my carbamazepine. No problems. You’re all too sensitive.