Medication Safety Risk Assessment
Answer a few quick questions to understand your risk of medication side effects based on your unique factors. This tool helps you identify if you might need more careful monitoring for your medications.
Your Medication Risk Assessment
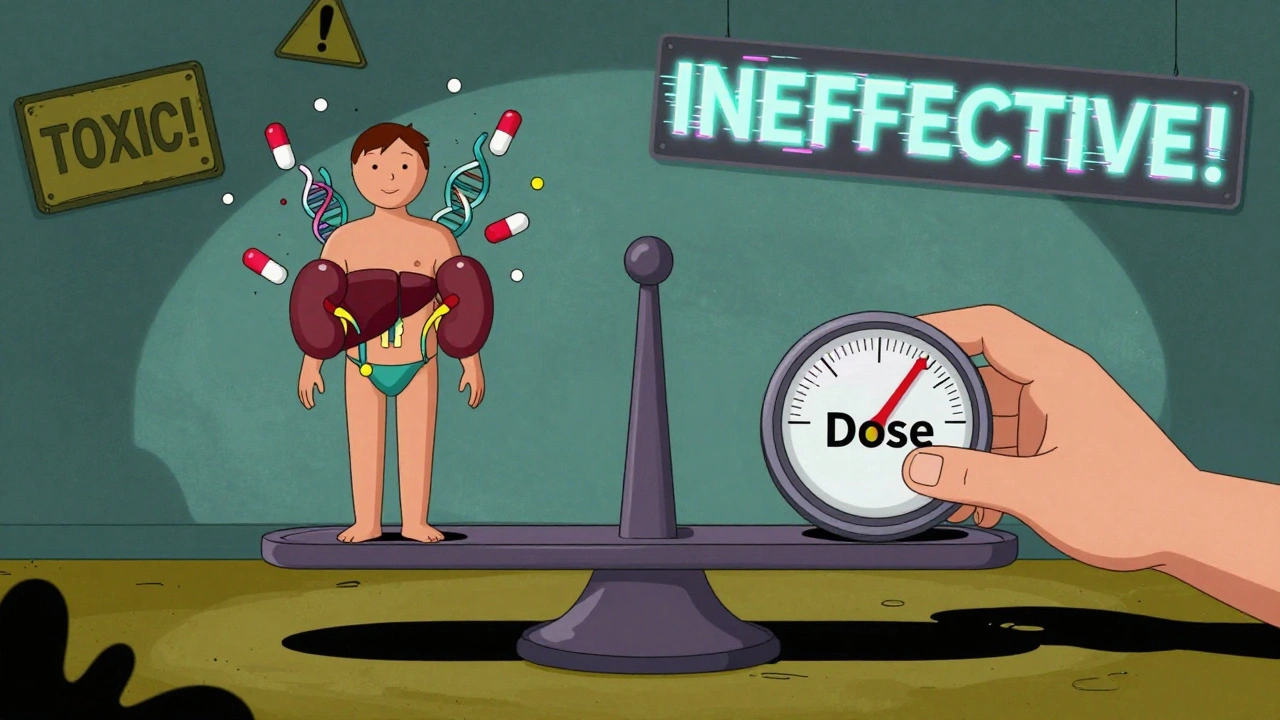
Getting the right dose of medication isn’t just about following the label. It’s about finding the sweet spot where the drug works without hurting you. Too little, and it does nothing. Too much, and you risk serious side effects-or worse. For many people, especially those on multiple medications or with chronic conditions, this balancing act is a constant, quiet struggle. The truth is, most prescriptions are written based on averages. But your body isn’t average. Your kidneys, your liver, your weight, your genes-they all change how a drug behaves in you. That’s why dose adjustment isn’t a one-time fix. It’s an ongoing conversation between you and your care team.
Why One Size Doesn’t Fit All
Think of your body like a car. Two people might drive the same model, but one fills up every 300 miles, the other every 400. Why? Driving habits, terrain, even the air temperature affect fuel use. Medications work the same way. A standard dose of warfarin might keep one person’s blood thin at the perfect level, while another person on the same dose could bleed internally or form a clot. That’s because of something called the therapeutic index. It’s the ratio between the dose that helps and the dose that harms. Drugs like digoxin, lithium, and phenytoin have a narrow therapeutic index-sometimes as low as 2 to 1. That means the difference between a safe dose and a toxic one is tiny. One extra pill, a change in diet, or a new antibiotic can push you over the edge.Who Needs Close Monitoring?
Not everyone needs frequent dose checks. But if you’re taking a Narrow Therapeutic Index (NTI) drug, you do. These include:- Warfarin (blood thinner)
- Digoxin (heart medication)
- Phenytoin (seizure control)
- Lithium (mood stabilizer)
- Cyclosporine (organ transplant rejection prevention)
The Hidden Risks of Polypharmacy
Taking five or more medications? You’re not alone. Nearly half of adults over 65 are. But the more pills you take, the higher your risk of bad interactions. One drug can block another’s metabolism, making it build up to toxic levels. Another might speed up clearance, making it useless. A study in Norwegian hospitals found that drug-related problems were far more common with NTI drugs-and most of those problems came from interactions, not just wrong doses. The American Academy of Family Physicians says this is one reason to regularly review your entire medication list. Ask your doctor: “Is every pill here still necessary?” Sometimes, cutting one or two drugs improves your health more than adding another.
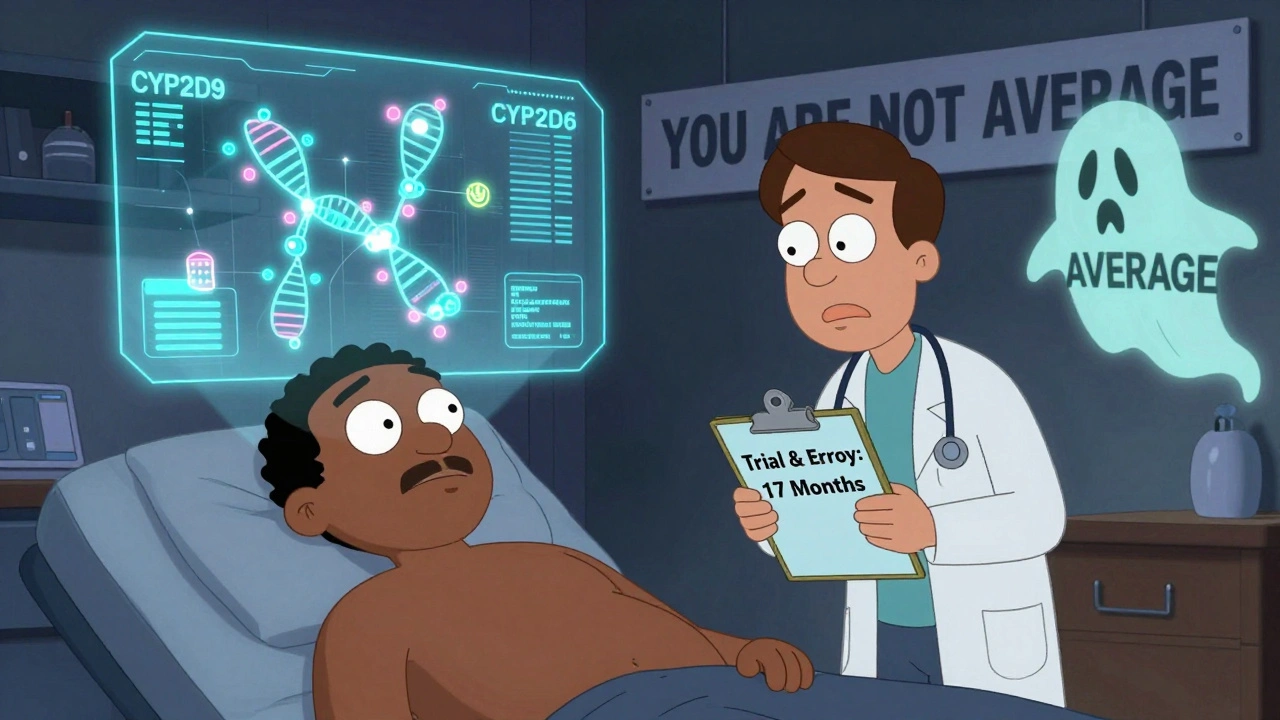
What Your Genetics Can Tell You
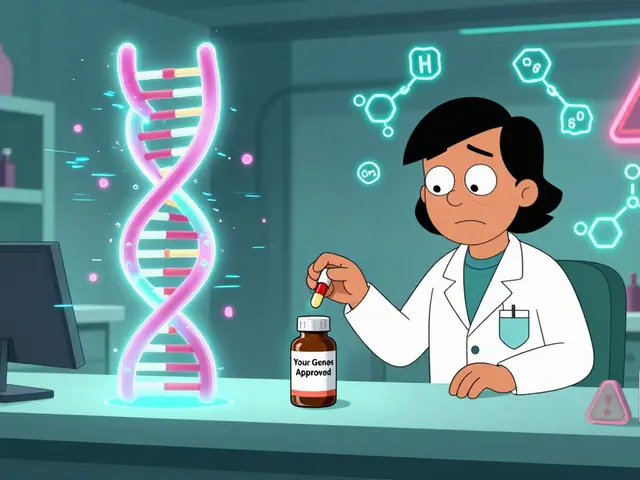
Your genes play a bigger role in how you respond to meds than most people realize. About 25% of commonly prescribed drugs are affected by genetic differences in how your body breaks them down. For example, some people have a variant in the CYP2C9 gene that makes them process warfarin extremely slowly. Give them the standard dose, and they’re at high risk of bleeding. Others have a CYP2D6 ultra-rapid metabolizer variant-they clear drugs like codeine so fast they get no pain relief, or worse, turn it into dangerous levels of morphine. Testing for these variants isn’t routine yet, but it’s becoming more common in hospitals and specialty clinics. If you’ve had bad reactions to meds in the past, or if your dose keeps changing, ask about pharmacogenomic testing. It’s not magic, but it can cut down the trial-and-error period from months to weeks.What You Can Do Right Now
You don’t need to wait for your doctor to bring this up. Here’s what you can do today:- Keep a real-time med list. Write down every pill, supplement, and herb you take-including doses and times. Update it after every doctor visit.
- Ask about monitoring. If you’re on an NTI drug, ask: “What lab tests do I need, and how often?” Don’t assume it’s being done.
- Know your kidney and liver numbers. Ask for your creatinine clearance or eGFR. If it’s below 60, your dose may need adjustment.
- Track side effects. Write down any new symptoms: dizziness, fatigue, nausea, rash, changes in heartbeat. Don’t brush them off as “just aging.”
- Ask about alternatives. If a drug has a narrow window and you’re struggling, ask: “Is there another medication with a wider safety margin?”
When to Suspect a Dose Problem
You don’t need a blood test to know something’s off. Watch for these red flags:- Feeling worse after a dose increase
- Symptoms returning after being stable for months
- Unexplained bruising, bleeding, or confusion
- Extreme fatigue or dizziness that started after a new prescription
- Missed doses because the schedule became too complicated
The Role of Pharmacists
Too many people see pharmacists as just the people who hand out pills. That’s a huge mistake. Pharmacists are trained in how drugs interact, how they’re processed in the body, and how to adjust doses based on real-world factors like age, weight, and organ function. Studies show that pharmacist-led dose management programs reduce medication errors by 35% and hospitalizations by 22% in older adults on multiple drugs. If your doctor isn’t adjusting your dose regularly, ask to speak with the pharmacy team. Many hospitals and clinics now have dedicated anticoagulation clinics for warfarin users, and they’ve cut major bleeding events by 60%. You don’t have to navigate this alone.The Future Is Personalized
The old model-give everyone the same dose based on a clinical trial of 500 healthy adults-is fading. The FDA and major research centers are pushing for precision dosing: using real-world data, genetic info, and AI to predict the right dose for you before you even start. Companies like InsightRX and DoseMe are already using algorithms that factor in 20 to 30 variables-kidney function, age, weight, genetics, other meds-to suggest optimal doses. In transplant centers, where survival depends on precise immunosuppressant levels, this is already standard. In primary care? Still rare. But it’s coming. The goal isn’t just to avoid side effects. It’s to make sure every dose you take actually helps.Final Thought: Your Dose Is Yours
Medication isn’t one-size-fits-all. Your body is unique. Your history, your genetics, your lifestyle-they all matter. Don’t accept a dose just because it’s on the label. Ask questions. Track your response. Push for monitoring if you’re on a high-risk drug. And don’t be afraid to say, “This isn’t working for me.” The right dose isn’t found by accident. It’s found by paying attention-and speaking up.What happens if I miss a dose of my medication?
It depends on the drug. For most medications, if you miss a dose by a few hours, take it as soon as you remember. But for NTI drugs like warfarin or digoxin, skipping or doubling up can be dangerous. Never double a dose unless your doctor tells you to. Instead, call your pharmacist or provider. They’ll help you decide what to do based on the specific drug, your condition, and how long you’ve missed the dose.
Can I adjust my own medication dose if I feel better or worse?
No. Even if you feel better, stopping or lowering your dose without medical advice can cause your condition to return-or worse, trigger withdrawal or rebound effects. If you feel worse, it could mean the dose is too high, too low, or interacting with something else. Never guess. Always consult your doctor or pharmacist before changing anything.
Are natural supplements safe to take with my prescription?
Not necessarily. Supplements like St. John’s Wort, garlic, ginkgo, and even grapefruit juice can interfere with how your body processes medications. St. John’s Wort, for example, can reduce blood levels of warfarin, making it less effective. Grapefruit juice can increase levels of statins and some blood pressure drugs, raising the risk of side effects. Always tell your pharmacist about every supplement you take-even if you think it’s harmless.
Why do some people need higher doses than others for the same drug?
Many factors affect this. Some people metabolize drugs faster due to genetics, liver function, or smoking. Others have slower kidney clearance, obesity, or age-related changes. A 70-year-old with reduced kidney function might need half the dose of a healthy 30-year-old. Even body composition matters-muscle vs. fat affects how drugs distribute in the body. There’s no universal rule. That’s why personalized dosing is so important.
How do I know if my medication dose is working?
For some drugs, it’s clear-you have less pain, lower blood pressure, or fewer seizures. But for others, like antidepressants or anticoagulants, the benefits aren’t always obvious. That’s why monitoring matters. Blood tests for INR, drug levels, or kidney/liver function tell you more than how you feel. If you’re stable and have no side effects, that’s a good sign. If symptoms return or new ones appear, it’s time to reassess.
Is it safe to take a lower dose if I’m worried about side effects?
It depends. For some drugs, like antibiotics or pain relievers, a lower dose might still work. But for NTI drugs like lithium or thyroid medication, even a small reduction can make the treatment ineffective. Never reduce your dose on your own. Talk to your provider. They might switch you to a different medication with a wider safety margin instead.
Can I get genetic testing to help with my medication dosing?
Yes, and it’s becoming more accessible. Tests like GeneSight or Pharmacogenomic Panels look at genes that affect how you process common medications. These are often used in psychiatry, cardiology, and pain management. Insurance doesn’t always cover them, but many clinics offer them as part of personalized care programs. Ask your doctor if it’s right for you-especially if you’ve had bad reactions to multiple drugs.
If you’re on multiple medications, especially high-risk ones, don’t wait for problems to arise. Start tracking your doses, ask about monitoring, and talk to your pharmacist. The right dose isn’t written in stone-it’s found through attention, communication, and smart questions.

Aileen Ferris
December 11, 2025 AT 06:19Frank Nouwens
December 11, 2025 AT 16:44Kaitlynn nail
December 12, 2025 AT 21:47Jack Appleby
December 13, 2025 AT 13:16Nikki Smellie
December 14, 2025 AT 16:39Michelle Edwards
December 15, 2025 AT 15:17Monica Evan
December 17, 2025 AT 01:37Taylor Dressler
December 18, 2025 AT 19:04Aidan Stacey
December 18, 2025 AT 23:39Jean Claude de La Ronde
December 19, 2025 AT 07:24Sarah Clifford
December 20, 2025 AT 12:39Paul Dixon
December 21, 2025 AT 04:09Ben Greening
December 21, 2025 AT 07:39Rebecca Dong
December 22, 2025 AT 07:30