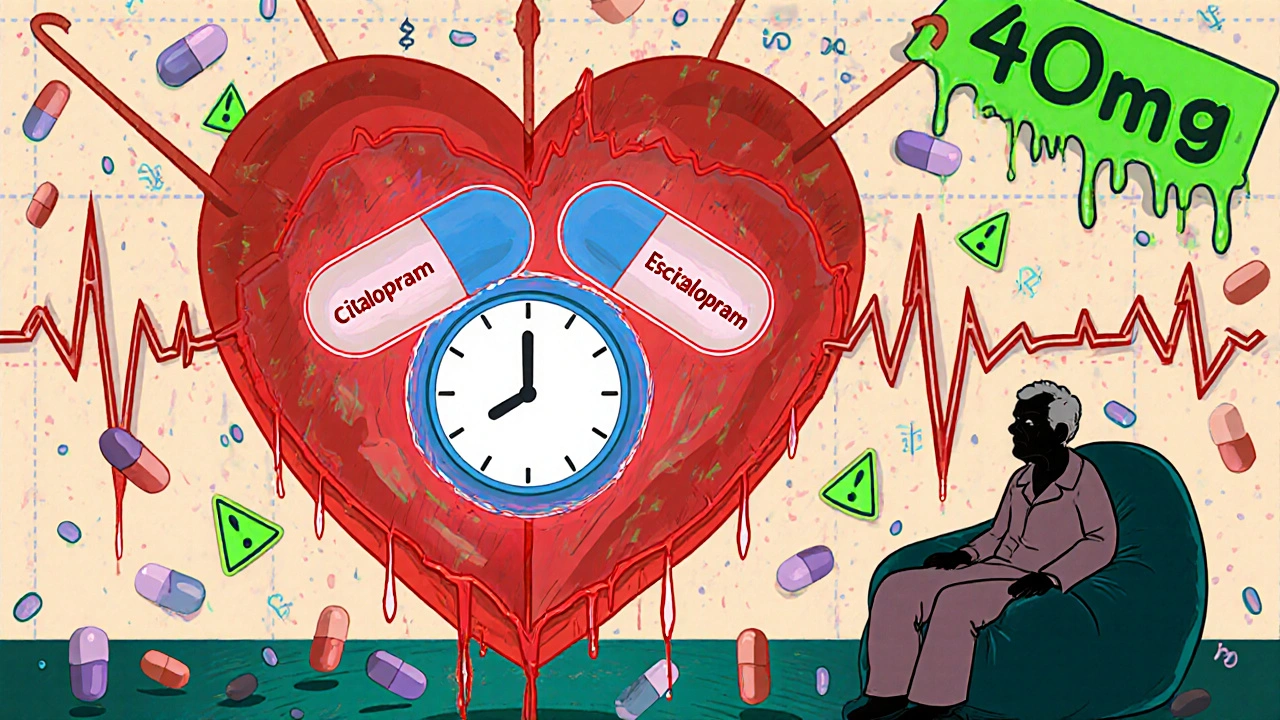
Citalopram QT Prolongation: Risks, Signs, and What You Need to Know
When you take citalopram, a selective serotonin reuptake inhibitor (SSRI) used to treat depression and anxiety. Also known as Celexa, it helps many people feel better—but it can also affect your heart in ways you might not expect. One of the most serious risks is QT prolongation, a change in the heart’s electrical cycle that can lead to irregular, potentially life-threatening rhythms. This isn’t something that happens to everyone, but if you’re on citalopram, you need to know the signs and who’s most at risk.
QT prolongation means the heart takes longer than normal to recharge between beats. On an EKG, it shows up as a longer QT interval. When this gets too long, it can trigger a dangerous rhythm called torsades de pointes. That’s rare, but it’s real. The risk goes up with higher doses of citalopram—especially above 40 mg a day. The FDA warns against doses higher than 40 mg for most adults, and 20 mg for people over 60 or those with liver problems. People with existing heart conditions, low potassium or magnesium, or those taking other drugs that affect the QT interval (like certain antibiotics, antifungals, or anti-nausea meds) are at higher risk. Even some over-the-counter antihistamines can add to the danger.
What should you watch for? Dizziness, fainting, fast or fluttering heartbeat, or sudden fatigue could be early signs. If you feel any of these, don’t wait. Get checked. It’s not about avoiding citalopram—it’s about using it safely. Your doctor should check your heart history before prescribing it, and may order an EKG if you’re at risk. Blood tests for electrolytes matter too. If you’ve been on citalopram for months without issues, that’s good—but it doesn’t mean you’re immune. Things change. New meds, dehydration, illness, or aging can shift your risk.
Some people worry about switching antidepressants because of this risk. But stopping suddenly is more dangerous. If you’re concerned, talk to your provider. There are other SSRIs and antidepressants with lower QT risk, like sertraline or escitalopram (which is actually the active part of citalopram). But the right choice depends on your whole health picture—not just one lab value.
Below, you’ll find real-world stories and expert guidance on how citalopram interacts with other drugs, what monitoring looks like, and how to spot trouble before it becomes an emergency. You’ll also see how this risk connects to other medications that affect the heart’s rhythm, and what to do if you’re on multiple drugs that could add up. This isn’t fear-mongering—it’s awareness. And awareness keeps you safe.