When you take a medicine like levothyroxine or tacrolimus, you’re not just taking a chemical-you’re trusting your body to stay within a razor-thin safety zone. These are NTI drugs-narrow therapeutic index medications. A tiny change in dose, or even a switch from one generic version to another, can push you from effective treatment into toxicity-or worse, leave you unprotected. For many patients, this isn’t theoretical. It’s daily reality.
What Makes a Drug an NTI Drug?
An NTI drug has a very small window between the dose that works and the dose that harms. Think of it like walking a tightrope. Step too far left, and your condition flares up. Step too far right, and you risk organ damage or even death. The therapeutic index measures this gap. For most drugs, it’s wide-maybe 10:1 or even 100:1. For NTI drugs, it’s often 2:1 or less.
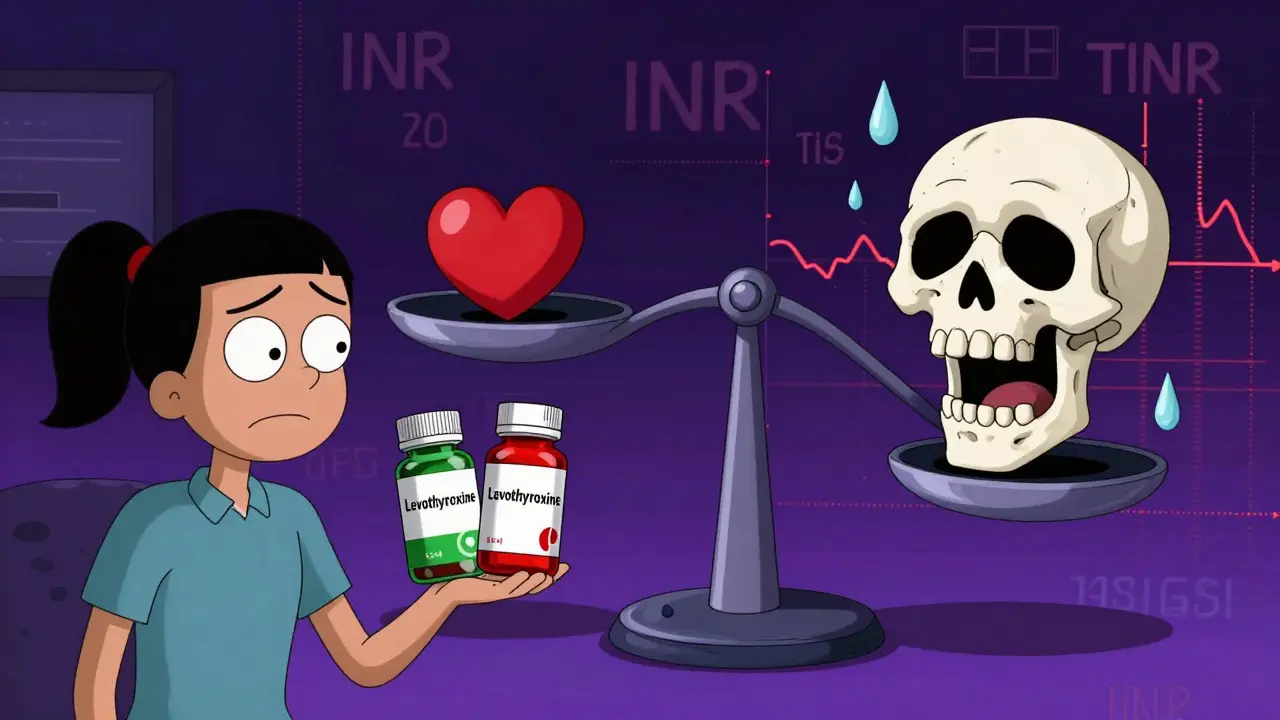
Take digoxin, used for heart failure. A dose that’s 10% too high can cause dangerous heart rhythms. Too low, and your heart keeps failing. Same with lithium for bipolar disorder. A slight rise in blood levels can cause tremors, confusion, or kidney damage. Warfarin, the blood thinner, has a therapeutic index of just 2-4. That means if your INR (a measure of blood clotting) goes from 2.5 to 3.5, you’re at much higher risk of bleeding. If it drops to 1.8, you’re at risk of a stroke.
The FDA doesn’t publish an official list, but it’s clear which drugs fall into this category: carbamazepine, phenytoin, cyclosporine, theophylline, valproic acid, and tacrolimus are all on the radar. These aren’t obscure drugs. Millions take them. And many are now available as generics.
Why Generic Switching Gets Complicated
The FDA says generic drugs are just as safe and effective as brand names. And for most drugs, that’s true. But for NTI drugs, the rules are stricter. The FDA requires bioequivalence testing with tighter limits: 95% to 105% for the active ingredient, compared to the standard 90% to 110%. Even then, small differences in how the drug is absorbed can matter.
One 2019 study looked at five generic versions of tacrolimus, used after organ transplants. The amount of active ingredient varied between 86% and 120% across brands. While none were outside FDA limits, the range was wide. In transplant patients, even a 10% drop in drug levels can trigger rejection. A 10% spike can cause kidney damage. These aren’t just numbers-they’re life-or-death margins.
Real-world data backs this up. A 2015 study of kidney transplant patients found that switching between different formulations of cyclosporine led to a 15.3% higher rate of acute rejection. Another study showed a 21.9% variation in tacrolimus blood levels when patients switched manufacturers. That’s not random noise-it’s a pattern. And for patients who’ve spent months stabilizing their levels, a switch can undo all that work.
What the Data Really Shows
Some studies say switching generics is fine. The FDA’s 2021 review of levothyroxine found no meaningful difference in TSH levels between brand and generic versions. The average difference was 0.03 mIU/L-statistically insignificant. That’s reassuring. But here’s the catch: 98.7% of patients stayed stable. That means 1.3% didn’t. For those people, it wasn’t a statistical anomaly. It was a crisis.
Pharmacists report something else: patient complaints. A 2019 national survey found that 63% of pharmacists had received reports from patients or doctors about problems after switching between generic manufacturers of NTI drugs. These aren’t rare. They’re common enough that doctors and pharmacists talk about them in hushed tones.
And it’s not just about blood levels. One study on warfarin showed that switching between generic manufacturers increased INR variability by 0.32 points. That’s small-but in a patient with atrial fibrillation, that’s enough to push them into the danger zone. The study didn’t find more bleeding events overall, but it didn’t need to. One extra bleed in a high-risk patient is one too many.
Why Doctors and Pharmacists Are Divided
There’s a gap between what the data says and what clinicians see. The American Medical Association said in 2007 that evidence against generic switching for NTI drugs was weak. But 82% of pharmacists surveyed said they almost always substituted generics for initial prescriptions. Meanwhile, 63% admitted they’d heard complaints about ineffectiveness or side effects after switching.
Neurologists are especially wary. The American Academy of Neurology recommends against automatic substitution of antiepileptic NTI drugs like carbamazepine and phenytoin. Why? Because even a small drop in blood levels can trigger a seizure. A patient might have been seizure-free for years-then after a pharmacy switch, they have a convulsion. No one wants that on their conscience.
And it’s not just about the drug. It’s about the patient. Someone on a stable dose of lithium for 10 years might handle a switch fine. Another person, with kidney issues or on multiple other meds, might not. There’s no one-size-fits-all.
State Laws and the Patchwork of Rules
Some states get it. Twenty-seven states have laws that restrict or require special consent before substituting NTI drugs. In those places, pharmacists must notify the prescriber or get permission before swapping a generic for another. In other states? It’s automatic. The patient doesn’t even know.
That’s a problem. If you’re on tacrolimus after a liver transplant, you don’t want your pharmacist to make a decision based on cost or convenience. You want your doctor to be in the loop. You want consistency. You want to know that the pill you’re taking today is the same as yesterday’s-even if it’s not the same brand.

What Patients Should Do
If you take an NTI drug, here’s what you need to do:
- Ask your doctor if your medication is an NTI drug. If they’re unsure, ask for the name and check the FDA’s product-specific bioequivalence guidance.
- Know your generic’s manufacturer. Write it down. Keep a note in your phone. If your pharmacy switches brands without telling you, ask why.
- Don’t assume “same drug = same effect.” Even if the label says “levothyroxine sodium,” the fill could be from a different factory. Ask for the same manufacturer every time.
- Get blood tests done regularly. If you’re on warfarin, check your INR. If you’re on tacrolimus, check your trough levels. Don’t wait for symptoms.
- If you feel different after a switch-fatigued, dizzy, having seizures, or your heart feels off-call your doctor immediately. Don’t wait. Don’t assume it’s “just in your head.”
What the Future Holds
The FDA is aware. Since 2018, they’ve required more in vivo studies for NTI drugs-meaning real human testing, not just lab simulations. They’re also tracking outcomes through post-market studies. So far, the data doesn’t show a widespread crisis. But that doesn’t mean it’s not happening for individuals.
What’s needed isn’t a ban on generics. It’s better communication. Better tracking. And respect for the fact that for some drugs, precision matters more than price.
For now, the safest approach is simple: if you’re on an NTI drug, stay on the same manufacturer. If you must switch, do it with your doctor’s approval-and monitor closely. Because when the margin between healing and harm is this thin, the right pill isn’t just a pill. It’s your safety net.
Are all generic drugs the same, even for NTI drugs?
No. While all generics must meet FDA bioequivalence standards, NTI drugs have tighter limits-and even within those limits, small differences in absorption can matter. Two generics of the same drug can have different fillers, coatings, or manufacturing processes that affect how quickly the drug enters your bloodstream. For most medications, that’s fine. For NTI drugs, it can be risky.
Can I switch between generic brands of levothyroxine safely?
Many patients can. FDA data shows that 98.7% of patients maintain stable TSH levels after switching. But 1.3% don’t. If you’ve been stable for years, switching might be fine. But if you’ve had recent changes in symptoms, weight, or energy, stick with the same manufacturer. Always check your TSH 6-8 weeks after a switch.
Why do some states restrict NTI drug substitution?
Because real-world reports show patients have had problems after switching-especially with seizure control, transplant rejection, or unstable INR levels. These laws give doctors and patients control over the switch, rather than leaving it to pharmacy policies or cost-saving measures. It’s about patient safety, not politics.
What should I do if my pharmacy switches my NTI drug without telling me?
Call your doctor right away. Ask if the new version is the same manufacturer as before. If not, request a refill with your original brand. Most doctors will support you. If your pharmacy refuses, ask to speak to the pharmacist-in-charge. You have the right to request the same manufacturer, especially for NTI drugs.
Is there a list of NTI drugs I can check?
The FDA doesn’t publish a single official list, but they’ve identified key NTI drugs in product-specific bioequivalence guidance. Common ones include warfarin, levothyroxine, lithium, phenytoin, carbamazepine, cyclosporine, tacrolimus, digoxin, and theophylline. Ask your pharmacist or doctor to confirm if your medication is on this list.


Arjun Seth
January 17, 2026 AT 09:53This is why generics are a scam! You think you're saving money, but you're playing Russian roulette with your life. One pill, different factory, and boom-you're in the ER. The FDA doesn't care. They're paid off by Big Pharma and Big Pharmacy. Wake up, people!
Ayush Pareek
January 18, 2026 AT 16:55I get where you're coming from, but not everyone reacts the same. My cousin switched generic levothyroxine and never noticed a difference. It's not black and white. The key is monitoring-check your labs, talk to your doctor, and don't panic over every switch. Stability matters more than the brand name on the bottle.
Jami Reynolds
January 20, 2026 AT 16:14Let me be perfectly clear: this isn't about bioequivalence-it's about corporate control. The FDA's 'tighter limits' are a joke. The same manufacturers produce both brand and generic versions under different labels. They're the same pills. The only difference? The price tag. And the silence from regulators is deafening.
Frank Geurts
January 22, 2026 AT 04:48As someone who has lived in five countries and seen healthcare systems from Tokyo to Toronto, I can say with confidence: the U.S. treats medication like a commodity, not a lifeline. In Germany, pharmacists must consult physicians before switching NTI drugs. In Japan, manufacturers are held to near-identical batch standards. Here? We gamble with organ rejection and seizures because of a 3-cent savings. It’s not just irresponsible-it’s immoral.
Dan Mack
January 22, 2026 AT 12:46They don't want you to know this but the FDA is in bed with the pharmacy benefit managers. They let companies switch generics without telling you because they want you to keep taking the same drug while they profit from the switch. You think your TSH is stable? Maybe. But your kidneys? Your liver? Your brain? That's a different story. They're watching you deteriorate slowly and calling it 'statistically insignificant.'
Amy Vickberg
January 23, 2026 AT 21:04I’ve been on cyclosporine for 12 years. I switched manufacturers twice-once without knowing-and I had a flare-up. I didn’t scream. I didn’t panic. I called my doctor, got my levels checked, and switched back. It’s not about fear. It’s about awareness. You don’t need a conspiracy. You just need to know your body and ask questions.
Nishant Garg
January 25, 2026 AT 20:20Look, in India, we don’t have the luxury of brand loyalty. We take what’s available, what’s affordable. But here’s the thing-my uncle on tacrolimus after his transplant? He got sick after a switch. We traced it to a new batch. He’s fine now, but it scared the hell out of us. So yes, consistency matters. But also, we’ve learned to test, track, and trust our own bodies more than any label. The system may be broken, but we’re still standing.
Nicholas Urmaza
January 26, 2026 AT 06:01Stop whining. If your drug isn't working, it's not the generic-it's you. Your metabolism, your diet, your stress levels. The science is clear. Most people are fine. The outliers? They're the ones who don't follow up. Get your blood drawn. Take responsibility. This isn't rocket science-it's basic healthcare hygiene.
Sarah Mailloux
January 27, 2026 AT 04:52My mom switched her levothyroxine and felt like a zombie for two weeks. We called the pharmacy-they didn't even tell her it changed. Now she keeps a photo of the pill on her phone and shows it to the pharmacist every time. Simple. Effective. No drama. Just smart.
Nilesh Khedekar
January 28, 2026 AT 02:04Oh wow, so the system is broken and you're surprised? Newsflash: capitalism doesn't care if you live or die as long as you keep buying pills. They'll switch your tacrolimus to the cheapest one, then charge you $500 for a blood test to fix what they broke. And you call that healthcare? I call it extortion with a stethoscope.