When you pick up a prescription, you might see two names on the bottle: one you recognize, like Lipitor, and another you’ve never heard of, like atorvastatin. One is expensive. The other costs a fraction of the price. But are they the same? The short answer is yes - and here’s why that matters.
They’re Not Just Similar. They’re the Same.
Generic drugs aren’t knockoffs. They’re not cheaper because they’re weaker or made with lower-quality ingredients. By law, they must contain the exact same active ingredient, in the same strength, and work the same way in your body as the brand-name version. The FDA requires every generic drug to prove it delivers the same amount of medicine into your bloodstream at the same speed as the original. That’s called bioequivalence - and it’s not a suggestion. It’s a hard rule.
For most drugs, the FDA allows a small range: 80% to 125% of the brand’s absorption rate. For drugs where even tiny differences matter - like blood thinners or thyroid meds - that range tightens to 90% to 111%. The FDA doesn’t approve generics unless they meet these standards. Thousands of studies back this up. In 2019, a JAMA Internal Medicine analysis of 38,000 patients on levothyroxine found no difference in outcomes between brand and generic versions. Same for blood pressure meds, cholesterol drugs, and diabetes treatments.
Why the Big Price Difference?
Brand-name drugs cost so much because the company that made them had to pay for years of research, clinical trials, and marketing before they could even sell it. Those costs get baked into the price. Once the patent expires - usually after 12 to 14 years - other companies can make the same drug. They don’t need to repeat expensive trials. They just need to prove their version works the same way. That cuts development costs by 90%.
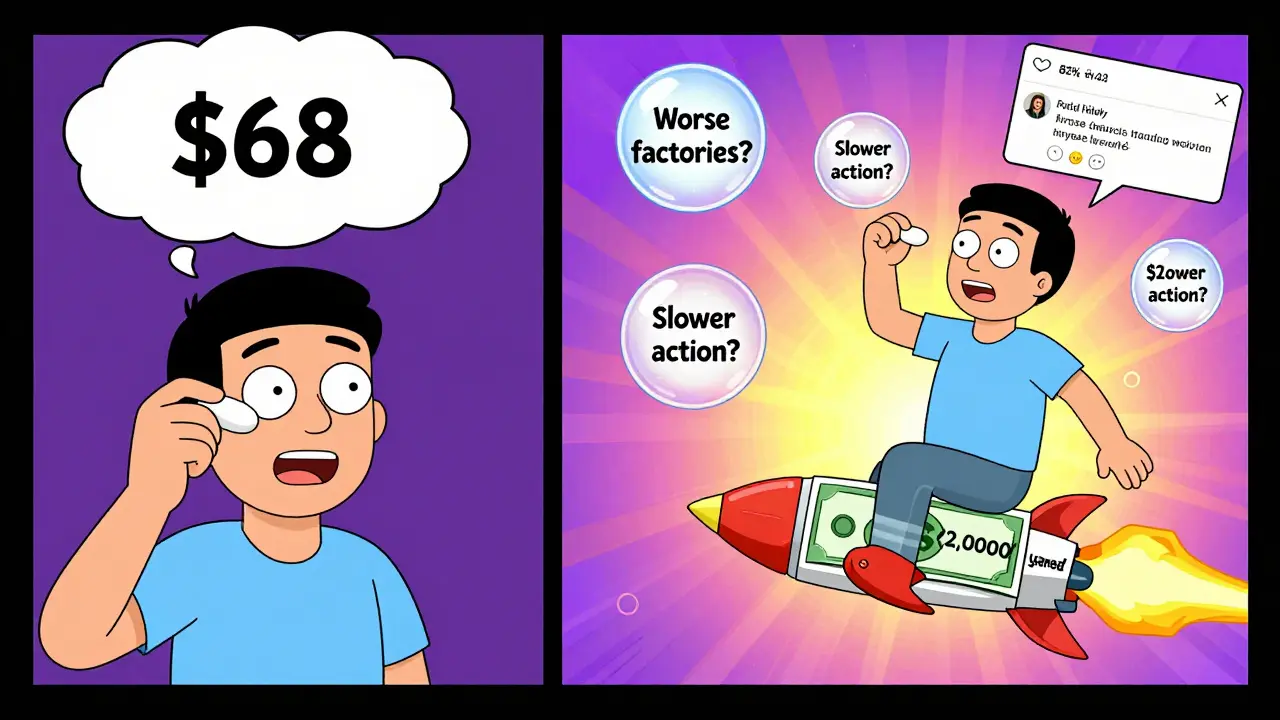
The result? Generics typically cost 80% to 85% less. In 2022, the average out-of-pocket cost for a generic prescription in the U.S. was $12.50. The brand-name version? $68.30. That’s not a small difference. For someone taking a daily pill for high blood pressure or diabetes, that adds up to over $2,000 a year in savings. The U.S. healthcare system saved $253 billion in 2022 just from generic drug use.
What’s Different? (And What’s Not)
Generics look different. They might be a different color, shape, or size. That’s not because they’re different inside - it’s because U.S. trademark laws say they can’t look exactly like the brand-name drug. You can’t have a generic version of a blue oval pill if the brand is a white capsule. So the generic might be a green oval instead. The inactive ingredients - things like fillers, dyes, or flavorings - might also change. But those don’t affect how the medicine works.
Some people worry that changing the filler could cause side effects. It’s rare, but it happens. If you’re allergic to a dye or lactose, you might react to one version and not the other. That’s why it’s important to check the inactive ingredients if you have known allergies. But for 99% of people, these differences are invisible.

When You Might Stick With Brand
There are exceptions. Some drugs have a narrow therapeutic index - meaning the difference between a helpful dose and a dangerous one is very small. Warfarin (a blood thinner), levothyroxine (for thyroid), and some seizure meds fall into this category. Because of that, some doctors prefer patients stay on the same version - brand or generic - to avoid even tiny fluctuations.
But here’s the twist: studies show those fluctuations rarely cause real problems. A 2022 Harvard Health review found that while some patients report feeling different after switching, most of those reports are psychological or due to other factors. In large, controlled studies, outcomes are nearly identical.
One Reddit user shared that their mom’s seizures got worse after switching from brand Lamictal to generic lamotrigine. She had to go back. That’s real. But out of hundreds of comments on that thread, only 14% reported similar issues. The rest - 86% - said they noticed zero difference in how the drug worked. That’s not luck. It’s science.
What You Can Do
If your doctor prescribes a brand-name drug, ask: "Is there a generic?" Most of the time, there is. Pharmacists are required by law in 49 states to substitute a generic unless the doctor writes "dispense as written" on the prescription. You don’t need to ask twice. The pharmacy will give you the cheaper option by default.
Keep a list of your meds - both brand and generic names. That way, if your prescription changes, you won’t be confused. GoodRx and other tools can show you price differences before you even walk into the pharmacy. Sometimes, even the generic version of a drug costs more at one pharmacy than another. It’s worth checking.
For chronic conditions - like diabetes, asthma, or high cholesterol - switching to generic can save you thousands over time. One person on Reddit saved $400 a month just by switching from brand Advair to its generic version. That’s not a one-time deal. That’s every month, for years.
The Bigger Picture
Generic drugs aren’t just a personal savings tool. They’re a public health win. In the U.S., 90% of all prescriptions filled are generics. But they make up only 25% of total drug spending. That means brand-name drugs, which make up just 10% of prescriptions, cost three times more than generics combined. That’s not efficient. It’s unsustainable.
From 2007 to 2016, generic drugs saved the U.S. healthcare system $1.67 trillion. That’s more than the annual GDP of many countries. The Congressional Budget Office estimates we’ll keep saving $200-$300 billion a year through 2030 - if generics stay accessible.
Right now, over 10,000 generic drugs are available for more than 2,000 brand-name medications. And that number is growing. Over 450 brand-name drugs are set to lose patent protection by 2028. That means even more options - and even more savings.
Myths Busted
- Myth: Generics are made in worse factories. Fact: The same companies often make both brand and generic versions. The FDA inspects all plants equally.
- Myth: Generics take longer to work. Fact: They’re required to reach the same blood levels at the same speed.
- Myth: If it’s cheaper, it must be less effective. Fact: Price doesn’t predict quality. The FDA doesn’t allow that.
There’s no magic in the brand name. It’s just a label. The medicine inside? That’s what matters.
What’s Next?
The FDA is working to speed up approval of complex generics - like inhalers, patches, and injectables - that have been harder to copy. The 2022 Inflation Reduction Act includes new rules to push more competition into the market. And the 2023 CREATES Act is trying to fix supply chain issues that caused shortages during the pandemic, when 80% of active ingredients came from just two countries: India and China.
For now, the message is simple: if your doctor says it’s okay, choose the generic. You’re not cutting corners. You’re making a smart, safe, and proven choice.




Elizabeth Cannon
January 23, 2026 AT 17:48Don Foster
January 24, 2026 AT 01:58Sushrita Chakraborty
January 24, 2026 AT 13:07Sawyer Vitela
January 26, 2026 AT 02:54Husain Atther
January 27, 2026 AT 10:37Helen Leite
January 27, 2026 AT 23:38Luke Davidson
January 29, 2026 AT 23:00asa MNG
January 31, 2026 AT 03:01Kevin Waters
January 31, 2026 AT 22:22Karen Conlin
February 2, 2026 AT 04:56