Imagine waking up one day and realizing you can’t walk like you used to. Your steps feel stuck, like your feet are glued to the floor. Then, you start forgetting where you put your keys-not just once, but often. And suddenly, you’re having accidents you never had before. You tell your doctor it’s just getting older. But what if it’s not? What if it’s something treatable?
That’s the story of normal pressure hydrocephalus, or NPH. It’s not dementia. It’s not Parkinson’s. It’s not just aging. It’s a hidden neurological condition that mimics them all-and yet, in most cases, it can be fixed. The key? Recognizing the signs early and knowing where to look.
What Exactly Is Normal Pressure Hydrocephalus?
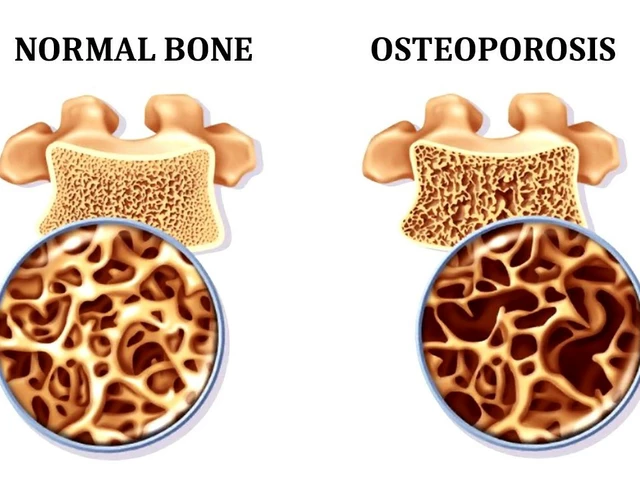
NPH is when too much cerebrospinal fluid (CSF) builds up in the brain’s ventricles. These are natural fluid-filled spaces that cushion the brain. In NPH, the fluid doesn’t drain properly, so the ventricles swell. But here’s the twist: the pressure stays normal. That’s why it’s called “normal pressure.” It’s not a sudden spike like in a stroke or trauma. It’s slow, quiet, and sneaky.
This condition mostly hits people over 60. About 1 in 250 adults over 65 have it, and in nursing homes, that number jumps to nearly 6 in 100. Yet, most never get diagnosed. Why? Because doctors often mistake it for Alzheimer’s or just old age.
The real tell? It’s not memory loss alone. It’s the combo. The classic triad: trouble walking, thinking slower, and losing bladder control. But here’s the catch-only about 30% of patients show all three at once. Most have one or two. And the first symptom? Almost always, it’s the gait.
The Gait That Doesn’t Look Like Anything Else
If you’ve seen someone with NPH walk, you’d notice something odd. Their feet don’t lift. They shuffle. Their stance is wide, like they’re trying not to fall. It’s called a “magnetic gait”-like their feet are stuck to the ground. They turn slowly, taking small, hesitant steps. They might bump into doorframes or trip on flat surfaces.
This isn’t like Parkinson’s, where tremors and stiffness dominate. It’s not like arthritis, where pain limits movement. NPH gait is a brain problem. It’s about the frontal lobes losing their grip on motor control. Studies show 100% of confirmed NPH patients have this gait issue. It’s the most reliable sign.
Doctors test it with a simple 10-meter walk. Time how long it takes. Measure stride length. Then, after a spinal tap removes 30-50 mL of CSF, do it again. If they walk faster, steadier, or longer after the tap, it’s a strong sign the shunt will help. A 10% improvement? That’s the magic number. It predicts shunt success 82% of the time.
Cognitive Changes That Look Like Dementia
Memory loss? Yes. But not the kind you think. In Alzheimer’s, people forget names, faces, recent events. In NPH, it’s different. It’s slower thinking. Trouble planning. Getting stuck on tasks. Forgetting why they walked into a room. They can’t juggle multiple steps-like making coffee while talking to someone.
Neuropsychological tests show this clearly. People with NPH struggle with the Trail Making Test Part B and Digit Symbol Substitution Test. These measure executive function and processing speed-skills controlled by the frontal lobes. That’s why they seem “lazy” or “unmotivated.” They’re not. Their brain can’t keep up.
And here’s the hopeful part: unlike Alzheimer’s, this isn’t permanent. In properly selected patients, up to 90% show cognitive improvement after shunt surgery. Some notice changes within days. One man on a patient forum said his mental fog lifted so fast he cried. He hadn’t felt clear-headed in two years.
Urinary Issues and the Other Missing Piece
Urinary incontinence shows up in about one-third of NPH cases. But it’s not always the first sign. Often, it’s the last. And it’s not about weak muscles. It’s about the brain losing its ability to signal when the bladder is full.
Patients describe sudden urgency. They can’t make it to the bathroom in time. Some wake up soaked at night. Others just leak a little. It’s embarrassing. It isolates people. Many stop leaving the house.
After shunt surgery, about 58% regain bladder control. That’s life-changing. No more diapers. No more fear. No more isolation. It’s one of the most rewarding outcomes for families.
How Do You Know It’s NPH and Not Something Else?
Here’s where things get tricky. NPH looks like Alzheimer’s. It looks like Parkinson’s. It looks like vascular dementia. But the differences matter.
- Alzheimer’s: Memory fades first. Gait stays normal until late. No sudden urinary issues. Brain scans show shrinkage, not swelling.
- Parkinson’s: Tremors, rigidity, slow movement-but gait is stiff, not magnetic. No CSF buildup.
- Vascular dementia: Symptoms come in steps, after strokes. Scans show multiple small strokes.
Imaging is key. An MRI or CT scan will show enlarged ventricles. The Evan’s index-a ratio of ventricle width to brain width-must be above 0.3. Periventricular white matter changes? Common. Aqueductal flow voids? Another clue.
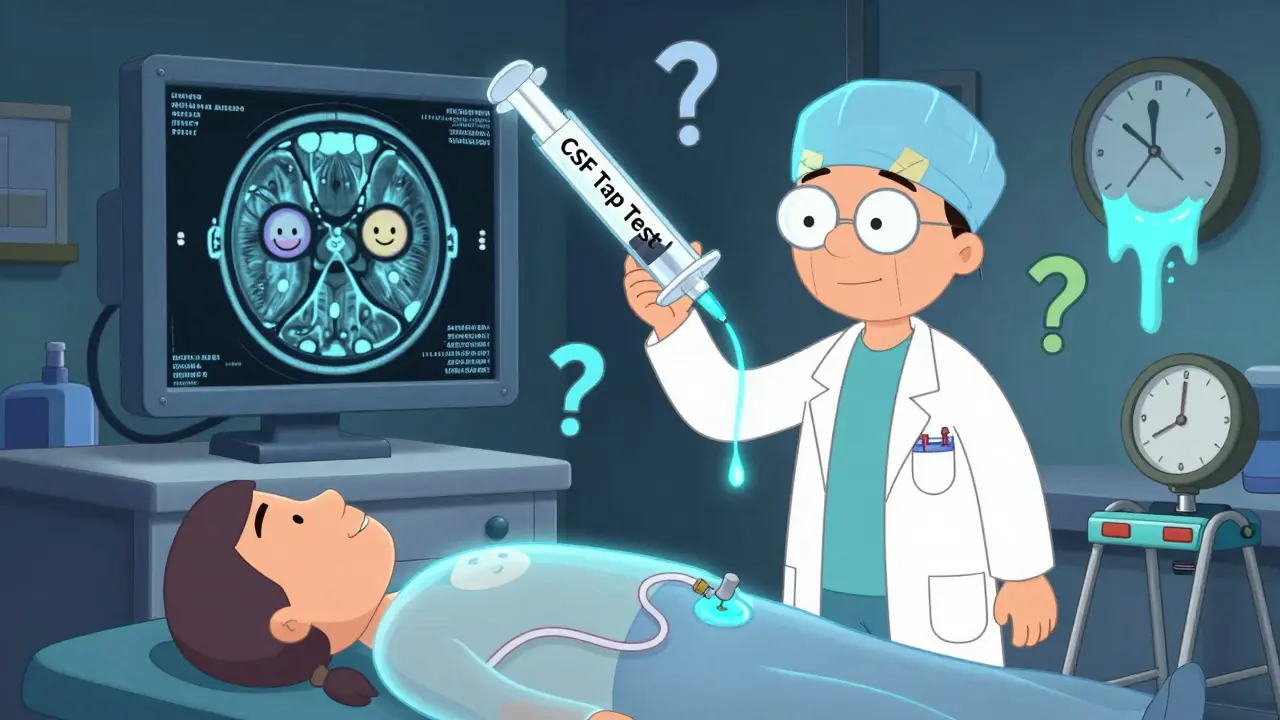
But the real test? The CSF tap test. Remove 30-50 mL of fluid. Wait an hour. Re-test walking and thinking. If there’s improvement? You’re looking at NPH. If not? Maybe it’s something else.
And here’s the sad truth: 60% of NPH cases are missed. Why? Because doctors don’t test for it. They assume it’s dementia. They don’t refer to neurosurgery. They don’t do the tap test.
The Shunt: How It Fixes the Problem
The only treatment for NPH is surgery. A shunt. It’s a thin tube. One end goes into the brain’s ventricle. The other goes down to the belly. A valve in between controls how much fluid drains.
It’s not a cure. But it’s a reset. The shunt doesn’t fix brain damage. It removes the pressure. Once the fluid drains, the brain can function again. Many patients say they feel like their old selves.
The procedure takes about an hour. General anesthesia. A small incision behind the ear. Another in the abdomen. Hospital stay: 2 to 7 days. Recovery: 6 to 12 weeks.
Success rates? 70-90% for the right patients. But not everyone improves. About 20-30% see little or no change. Why? Maybe they waited too long. Maybe they had other brain changes mixed in. Or maybe the shunt didn’t work right.
What Can Go Wrong After Surgery?
Shunts aren’t perfect. They can get infected. About 8.5% of patients do. They can clog. About 15% need a revision within two years. Some develop bleeding in the brain-subdural hematomas-in 5.7% of cases.
Over-drainage is another risk. Too much fluid leaves the brain. It can cause headaches, nausea, or even collapse. Under-drainage? The fluid builds back up. Symptoms return.
That’s why follow-up is critical. Check-ins at 2 weeks, 6 weeks, 3 months. Adjustments to the valve pressure may be needed. Some valves are programmable-doctors can tweak them with a magnet outside the skin. No extra surgery.
Older patients-over 80-have higher infection rates. Insurance doesn’t always cover the tests. One patient said she waited 18 months because her insurer denied the lumbar puncture. That delay cost her months of recovery time.

Who Benefits Most? Who Doesn’t?
Not everyone is a good candidate. The best candidates:
- Have clear gait disturbance as the first symptom
- Show improvement after a CSF tap test
- Are under 80 years old
- Have no major strokes or severe Alzheimer’s changes on MRI
- Got diagnosed within 12 months of symptoms starting
Delay hurts. If you wait more than a year, the chance of improvement drops by 30%. That’s why speed matters.
Patients with mixed conditions-like NPH plus early Alzheimer’s-do worse. Their cognitive gains are smaller. But gait and bladder often still improve. And that’s still life-changing.
What’s New in NPH Diagnosis and Treatment?
There’s hope on the horizon. In 2022, the FDA approved a new device called the Radionics® CSF Dynamics Analyzer. It measures how well fluid drains from the brain-something MRI can’t do. It’s improving diagnostic accuracy to 89%.
There’s also a new app, the iNPH Diagnostic Calculator. You plug in 12 symptoms and test results. It tells you the chance of shunt success. It’s 85% accurate.
Researchers are testing blood and CSF biomarkers. In early trials, a simple fluid test can spot NPH with 92% accuracy. No tap. No MRI. Just a blood draw. That could change everything.
And the shunts themselves? Better. Modern valves are programmable, infection-resistant, and last longer. But they still need monitoring. The average shunt lasts 6.3 years before needing repair.
Real Stories, Real Results
A 72-year-old man in Ohio had been using a walker for 18 months. He couldn’t climb stairs. He wet his pants daily. After the tap test, he walked 10 meters in 12 seconds instead of 28. He got a shunt. Within 48 hours, he was walking without help. Within a week, he was back to gardening.
A 68-year-old woman in Minnesota had the tap test. She improved. She got the shunt. But her memory didn’t get better. She got headaches. She needed a valve adjustment. She says she’d do it again-because she could walk, and that mattered more than the memory.
Of 457 patients surveyed by the Hydrocephalus Association, 76% saw better walking. 62% felt sharper. 58% regained bladder control. 89% said they were glad they did it-even if they had complications.
The biggest complaint? The wait. On average, people wait 14 months from first symptom to diagnosis. That’s 14 months of lost independence. Of shame. Of fear.
Don’t wait. If you or someone you love has unexplained gait trouble, forgetfulness, or bladder issues-ask for a CSF tap test. Ask for an MRI. Ask for a neurosurgery consult. It’s not normal aging. It might be NPH. And it might be fixable.
Is normal pressure hydrocephalus the same as dementia?
No. NPH mimics dementia but is different. Alzheimer’s causes memory loss first, with walking problems late. NPH starts with trouble walking, then thinking, then bladder control. The big difference? NPH can be reversed with surgery. Alzheimer’s cannot.
Can NPH be diagnosed without surgery?
Yes. The CSF tap test-removing 30-50 mL of spinal fluid-is the gold standard for predicting shunt success. If walking or thinking improves after the tap, surgery is likely to help. MRI and CT scans also show enlarged ventricles and other signs without needing surgery.
How long does it take to recover from a shunt surgery?
Most people leave the hospital in 2-7 days. Full recovery takes 6-12 weeks. Gait often improves within days. Cognitive changes may take weeks to months. Bladder control can improve in as little as a week or take longer. Patience is key.
Are shunts permanent?
Shunts are meant to be long-term, but they aren’t foolproof. About 15% need revision within two years due to blockage or infection. Most last 5-7 years. Modern programmable valves can be adjusted without surgery using a magnet. Regular follow-ups are essential.
Why is NPH often misdiagnosed?
Because its symptoms look like aging, Alzheimer’s, or Parkinson’s. Doctors don’t always think to test for it. The CSF tap test isn’t routine. Insurance often denies it. Many patients are told it’s “just getting older.” But NPH is one of the few treatable causes of dementia-like symptoms. Asking for the test could change everything.



Tracy Howard
January 19, 2026 AT 11:37Oh for god's sake, another one of these 'it's not aging' clickbait articles. My aunt had this 'NPH' nonsense and they stuck a shunt in her like she was a broken faucet. Three months later, she was in a nursing home with a UTI and a collapsed lung. Don't you dare call it 'fixable'-it's a gamble with a 30% failure rate and a 15% chance your loved one dies on the table. And don't get me started on the cost. Insurance won't cover the tap test unless you're rich or Canadian. Which, by the way, we are. And we still had to fight.
Aman Kumar
January 20, 2026 AT 10:43Let me elucidate the pathophysiological underpinnings: NPH is not a standalone entity but rather a downstream epiphenomenon of impaired glymphatic clearance in the context of age-related perivascular space dilation. The CSF tap test is a crude proxy for aqueductal flow dynamics, yet neurosurgeons treat it as gospel. Modern biomarkers like CSF tau/p-tau ratios and amyloid-β42/40 indices are far more predictive-but of course, you won't find those in a Reddit post written for the cognitively impaired demographic. The real tragedy? The shunt industry is a $1.2B market. They don't want you to know it's often just cerebral atrophy masquerading as NPH.
Jake Rudin
January 21, 2026 AT 05:38It's fascinating-this condition, this quiet, creeping collapse of motor intentionality-how it mirrors the collapse of meaning in late modernity. We mistake the body's decline for the soul's. We say 'it's just aging,' and we look away. But here, in this triad-gait, cognition, continence-we see not decay, but disconnection. The brain isn't broken-it's drowning in its own silence. And the shunt? It's not a cure. It's a whisper back into the world. A single drop of CSF removed, and suddenly, a man remembers how to hold his wife's hand. Isn't that what we're all begging for? To be heard, even when we can't speak?
Lydia H.
January 22, 2026 AT 20:08My dad had this. He was 74. We didn't know what was wrong for 18 months. He stopped gardening. Stopped laughing. Started forgetting his own birthday. Then one day, my mom begged the neurologist for the tap test. They said 'probably dementia.' She said 'try it anyway.' He walked out of the hospital two days later without his cane. He cried. I cried. He lived another 5 years-clear-headed, dancing in the kitchen, telling terrible jokes. This isn't a miracle. It's a basic test. Why isn't it standard?
Astha Jain
January 23, 2026 AT 17:36OMG i had no idea this was a thing!! My grandpa was like this, we thought he was just senile… but now i think maybe he had this?? i mean like, he would just stare at the fridge like it was a puzzle?? and then he'd pee his pants and say 'oh i forgot'… like?? why didnt anyone test him??
Phil Hillson
January 25, 2026 AT 05:52So let me get this straight-some guy shuffles, forgets his keys, and suddenly you want to drill a hole in his skull and install a plumbing system? This isn't medicine. This is a horror movie. And the author acts like this is a miracle cure. Newsflash: 20-30% of people get worse. Some get brain bleeds. Some end up in a coma. And you're just gonna hand out shunts like candy? This isn't science. It's desperation dressed up in MRI images.
Erwin Kodiat
January 26, 2026 AT 03:32I'm from the Philippines and we don't have access to shunt surgery for most people. But I've seen elderly relatives with these symptoms. They sit. They don't move. They don't speak. No one calls it NPH. They just call it 'old.' I wish this post had been around when my lolo was alive. He could've walked again. I hope someone reading this goes to their doctor and asks for the tap test. Don't wait. Don't assume. Ask.
Valerie DeLoach
January 27, 2026 AT 12:09Thank you for writing this with such clarity and compassion. Too often, neurology reduces people to symptoms. But here, you’ve honored the humanity behind the triad. I’m a geriatric nurse practitioner, and I’ve seen the shame in patients’ eyes when they can’t control their bladder. I’ve seen the quiet resignation when they’re told, ‘It’s just aging.’ This post isn’t just medical-it’s moral. Please share it with every primary care clinic, every senior center, every nursing home. We owe it to our elders to know better.
Christi Steinbeck
January 27, 2026 AT 15:09STOP WAITING. If your parent, grandparent, spouse-anyone you love-is shuffling, forgetting, or leaking-DON’T WAIT. Go to the ER. Demand a CT scan. Ask for a neurosurgeon. Tell them you’ve read this. Tell them you’re not accepting ‘it’s just aging.’ I’m not being dramatic. I’ve seen people die because no one listened. You have power. Use it. Now. Your loved one deserves to walk again.
Jacob Hill
January 29, 2026 AT 11:55Just wanted to say-I had a cousin who got the shunt. He improved dramatically. But the valve got infected. Then it clogged. Then he needed a second surgery. Then the battery in the programmable valve died. He’s been on six revisions in eight years. So yes, it works. But it’s not a one-and-done miracle. It’s a lifelong maintenance nightmare. I’m glad he walks again. But I’m also terrified for anyone else who might think this is easy.
Josh Kenna
January 30, 2026 AT 14:02Bro this is wild I had no idea this was a thing my uncle had this and they told him he was just getting old and now he's dead and I think if they had just done the tap test he'd still be here like I'm not even mad I'm just heartbroken why does no one know about this why is this not on every doctor's checklist why why why
Lewis Yeaple
January 31, 2026 AT 13:48It is imperative to note that the diagnostic criteria for idiopathic normal pressure hydrocephalus, as defined by the 2005 International Society for NPH Guidelines, require the presence of all three components of the classic triad, corroborated by neuroimaging and CSF dynamics. The assertion that 30% of patients exhibit the full triad is misleading; in fact, the presence of even two components, in conjunction with radiological evidence and a positive tap test, constitutes a probable diagnosis. The cited 82% predictive value for shunt success is derived from prospective cohort studies with strict inclusion criteria, and should not be extrapolated to heterogeneous populations without proper neurologic evaluation.
Jackson Doughart
January 31, 2026 AT 16:52I used to work in neurosurgery. I saw the shunts go in. I saw the tears when they came out. I saw the ones who didn’t make it. I saw the ones who came back-alive again, not just alive. I never told families it was a cure. I told them it was a second chance. A quiet one. A fragile one. But real. If you’re reading this, and someone you love is fading-don’t let them fade quietly. Ask. Push. Fight. Even if it’s just for one more walk. One more laugh. One more moment before the silence takes them. It’s worth it.