Medication Safety and Side Effects in November 2025: Statins, NTI Drugs, and More
When it comes to medication safety, the practice of using drugs correctly to avoid harm while getting the intended benefit. Also known as drug safety, it’s not just about taking pills on time—it’s understanding what your body is reacting to, when to speak up, and how to spot hidden risks before they become emergencies. In November 2025, patient reports and new research highlighted that even common medications like statins, cholesterol-lowering drugs often prescribed long-term can disrupt sleep, causing insomnia or vivid dreams, especially lipophilic ones like simvastatin. While large studies dismiss these effects, real-world experiences show they’re real—and manageable with timing changes or switching brands.
Another major focus was narrow therapeutic index drugs, medications where the difference between a helpful dose and a dangerous one is razor-thin. Drugs like warfarin, lithium, and levothyroxine fall into this category. Switching from brand to generic—or even between generic brands—can throw blood levels out of range, leading to toxicity or treatment failure. That’s why drug monitoring, the process of measuring drug levels in the blood to ensure safety and effectiveness isn’t optional for these patients. It’s essential. And it’s not just about blood tests—it’s about knowing when to ask your pharmacist or doctor if a new pill is truly the same as the last one.
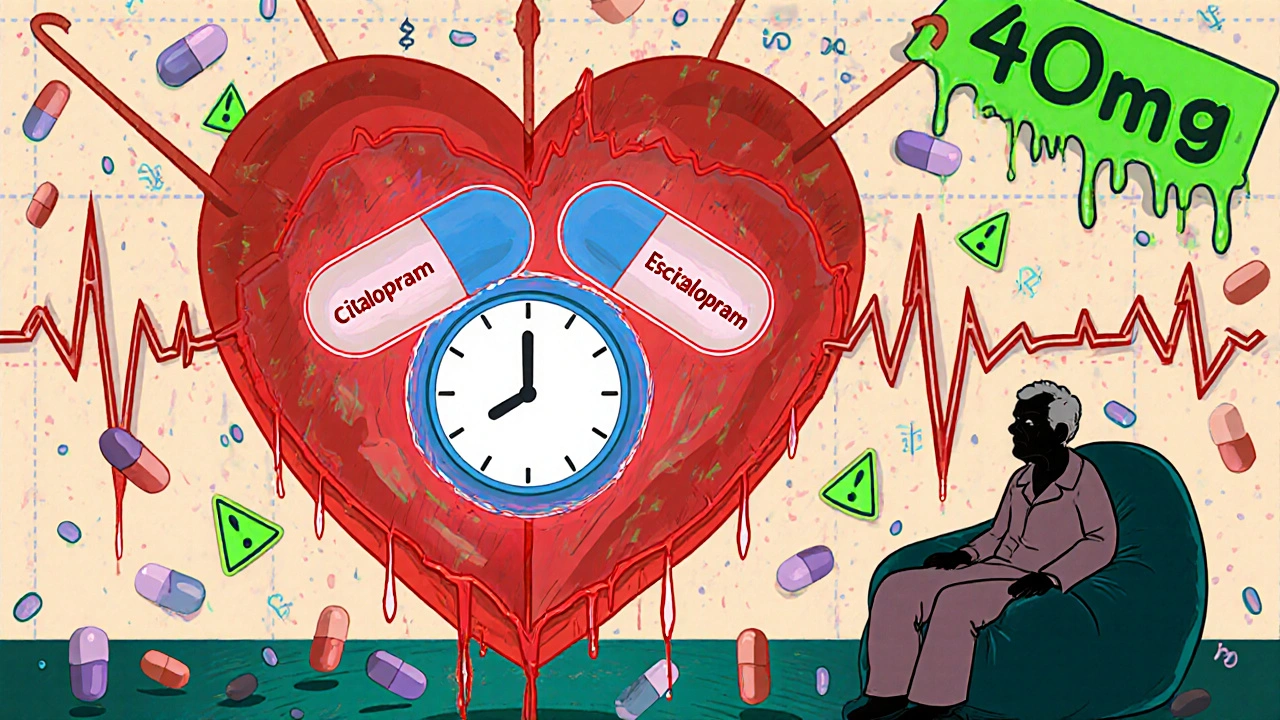
Then there’s the quiet danger of anticholinergic burden, the cumulative effect of drugs that block acetylcholine, a key brain and nerve chemical. Tricyclic antidepressants like amitriptyline are common culprits. They might help with depression or nerve pain, but over time, they’re linked to memory fog, confusion, and even higher risk of dementia. The scary part? Many of these effects reverse once the drug is stopped. Yet patients often stay on them because no one ever explained the trade-off.
These aren’t isolated issues. They’re connected. A patient on a beta blocker for glaucoma might also be taking a statin and a thyroid pill—all of which need careful tracking. Someone using an opioid patch for chronic pain could be at risk of accidental overdose if they don’t know how to dispose of it safely. And generics? They’re not always interchangeable. Allergic reactions to dyes or fillers in generic versions can be just as serious as reactions to the active ingredient.
What you’ll find in this collection isn’t theory. It’s what real people are dealing with: how to read medication guides to spot red flags, how to report a dosing error before someone gets hurt, why patching therapy for lazy eye works better the earlier it starts, and how to protect your hearing from drugs you didn’t even know could damage it. These posts don’t just list risks—they give you clear steps to take control. Whether you’re managing Parkinson’s, IBD, or just trying to remember to take your pills, the tools here are practical, updated, and built for people who need answers—not jargon.